Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Sclerosis and Related Disorders – Clinical Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
ANCA are detected in 0-11.7% (1) of patients with systemic sclerosis (SSc) and only a minority of these patients will develop an overlap syndrome with ANCA associated vasculitis (AAV). The clinical significance of ANCA in SSc patients without AAV is unknown. The aim of this study was to determine the prevalence of ANCA in a large SSc cohort and the association between ANCA positivity and SSc clinical characteristics, autoantibodies and mortality.
Methods:
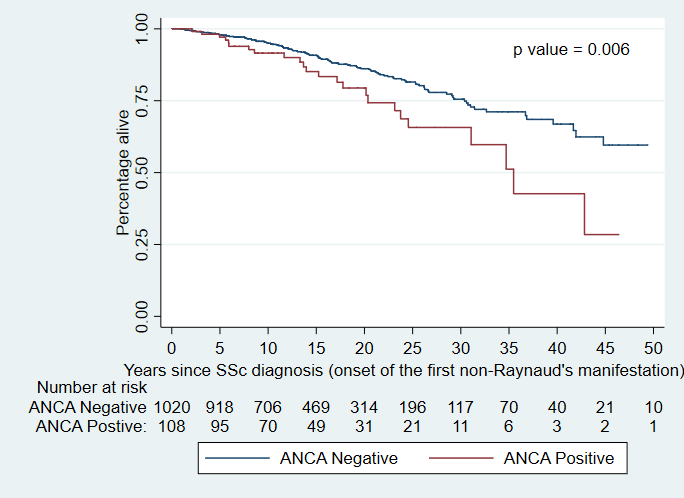
The cohort comprised patients who fulfilled 2013 ACR/EULAR criteria for SSc, enrolled in a multicentre prospective cohort study across 13 centres. ANCA positive (ANCA+) was defined as the presence of at least one of p-ANCA, c-ANCA, atypical ANCA, MPO or PR3. Univariable and multivariable associations of ANCA were determined using Chi-square and logistic regression. The effect of ANCA status on mortality was studied using Kaplan Meier survival analysis.
Results:
Of 1303 patients who fulfilled inclusion criteria, 116 (8.9%) were ANCA+. Median follow-up was 3.5 years (IQR 2.7). Mean ± SD age at recruitment was 57.7 ± 12.5 years and 25.2% had diffuse SSc. Of the ANCA+ group, 2 (1.7%) had AAV, 13 (11.2%) were MPO+ and 18 (15.5%) were PR3+. Gender and disease subtype did not significantly differ between the ANCA+ and ANCA- groups. The ANCA+ group had a higher prevalence of Asian patients (12.9% vs 3.7%, p=0.001), interstitial lung disease (ILD) (44.8% vs 21.8%, p<0.001), malignancy (26.7% vs 18.6%, p=0.04), synovitis (54.3% vs 38.2%, p=0.001), overlap syndrome with Sjogren’s (4.3% vs 1.6%, p=0.04), and overlap features with another connective tissue disease (12.1% vs 5.2%, p=0.003). Pulmonary embolism (PE) was more common among ANCA+ patients (8.6% vs 3.0%, p=0.002) even after adjusting for antiphospholipid antibodies. ANCA+ patients had a higher prevalence of anti-Scl70 (25.0% vs 12.8%, p<0.001) and anti-Ro (11.2% vs 6.2%, p=0.04). ILD remained significantly associated with ANCA in multivariable analysis adjusting for anti-Scl70 (OR 2.6, 95%CI 1.7-4.0, p<0.001). Use of azathioprine (13.8% vs 7.5%, p=0.017) and calcium channel antagonists (75% vs 64%, p=0.018) was more common in the ANCA+ group. The PR3+ group was more likely than PR3- to have anti-Scl70 (44.4% vs 13.4%, p<0.001), ILD (50% vs 23.4%, p=0.009), PE (16.7% vs 3.3%, p=0.022) and to use mycophenolate (22.2% vs 7.6%, p=0.046). The MPO+ group was more likely than MPO- to have anti-Scl70 (38.5% vs 13.6% p=0.006), overlap syndrome with rheumatoid arthritis (15.4% vs 1.9%, p=0.028) and to use cyclophosphamide (30.8% vs 8.8%, p=0.023). ANCA+ patients had higher mortality than ANCA- patients (p=0.006).
Conclusion:
In SSc, ANCA identifies a high risk group, with greater prevalence of ILD and PE, and poorer overall survival. ANCA+ SSc patients require close monitoring for complications.
1. Quéméneur T, et al. Systemic Vasculitis During the Course of Systemic Sclerosis. Medicine (Baltimore) 2013;92.
To cite this abstract in AMA style:
Moxey J, Huq M, Proudman S, Sahhar J, Ngian GS, Walker J, Strickland G, Wilson M, Ross L, Major G, Roddy J, Stevens W, Nikpour M. Significance of Anti-Neutrophil Cytoplasmic Antibodies in Systemic Sclerosis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/significance-of-anti-neutrophil-cytoplasmic-antibodies-in-systemic-sclerosis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/significance-of-anti-neutrophil-cytoplasmic-antibodies-in-systemic-sclerosis/