Session Information
Date: Tuesday, October 23, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster III: Treatment
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Osteoporosis is common in patients with systemic lupus erythematosus (SLE). Guidelines for the treatment and prevention of glucocorticoid induced osteoporosis (GIOP) are detailed for postmenopausal women and older men. However, there are less data on risk factors for osteoporotic fracture in premenopausal women and men < 50 years old with SLE resulting in conditional recommendations in the 2017 American College of Rheumatology GIOP guidelines. The goal of this project is to identify risk factors for osteoporotic fracture in premenopausal women and men < 50 with SLE.
Methods:
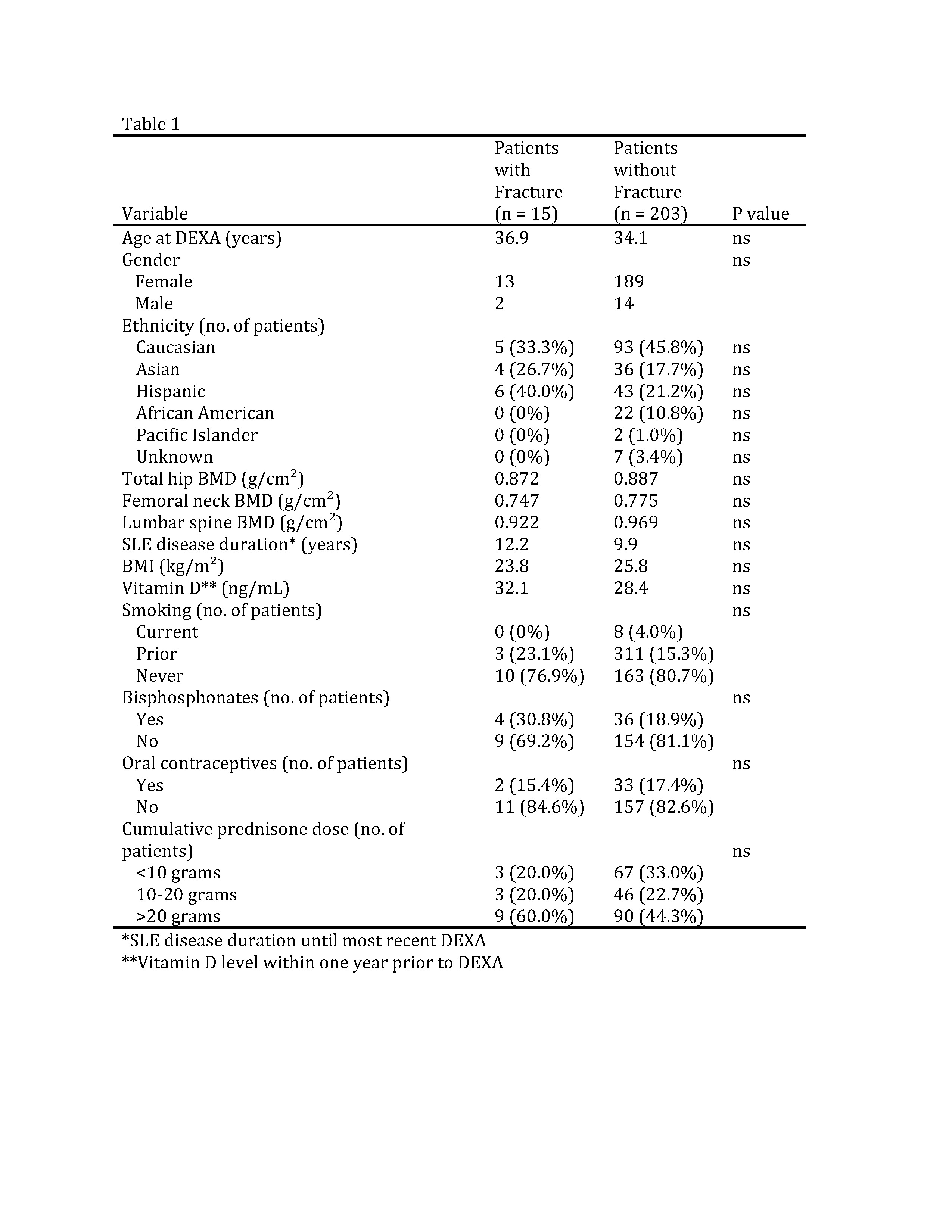
In this retrospective chart review of SLE patients at an academic medical center, 218 premenopausal women (defined as age < 45 or age at menopause) and men (age < 50) with bone mineral density (BMD) results were identified. All patients fulfilled the 1997 ACR criteria for the classification of SLE. Variables collected included BMD, osteoporotic fracture (rib, sacrum, hip, spine, wrist, forearm, humerus, ankle, tibia/fibula fractures1), smoking, BMI, gender, SLE disease duration, bisphosphonate and oral contraceptive (OCPs) use, ethnicity, age, vitamin D, and lifetime cumulative prednisone dose categorized as <10, 10-20, and >20 grams. Variables were collected at the time of BMD or fracture. The fracture and non-fracture groups were compared using Student’s t-test for continuous variables and chi-squared test for categorical variables. Multivariate analysis was used to examine potential variables associated with fracture.
Results:
This study included 202 women and 16 men who had a mean age of 34.5 years. Out of the 218 subjects, 15 (2 men, 13 women) had an osteoporotic fracture. One subject had 2 fractures. Fractures included 2 tibia, 2 forearm, 1 ankle, 2 rib, 1 hip, and 8 vertebral. No difference was found in BMD of the lumbar spine, hip, or femoral neck between those with fracture vs no fracture. Lifetime cumulative prednisone dose, BMI, smoking, vitamin D level, use of bisphosphonates or OCPs, gender, ethnicity, and SLE disease duration were not associated with increased risk of fracture. In those with fracture, 9 had used >20g of cumulative lifetime prednisone use, 3 had used 10-20g, and 3 <10g; however, these findings did not reach statistical significance. There were no associations between fracture and age, lumbar BMD, cumulative prednisone dose, ethnicity, or BMI on multivariate analysis.
Conclusion:
Osteoporotic fractures were infrequent (6.9%) in premenopausal women and men < 50 with SLE, but higher than would be expected in a healthy population. There was no significant association between fracture risk and BMD nor cumulative prednisone dose highlighting a need for further studies to determine risk factors to identify patients most likely to benefit from preventive osteoporotic medications.
- Warriner AH, Patkar NM, Curtis JR et al. Which fractures are most attributable to osteoporosis? J Clin Epidemiol. Jan 2011;64(1):46-53.
To cite this abstract in AMA style:
Driver T, McMahon MA, Tsao B, Grossman JM. Bone Mineral Density Is Not Associated with Osteoporotic Fractures in Premenopausal Women and Men < 50 Years Old with Systemic Lupus Erythematosus [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/bone-mineral-density-is-not-associated-with-osteoporotic-fractures-in-premenopausal-women-and-men-50-years-old-with-systemic-lupus-erythematosus/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/bone-mineral-density-is-not-associated-with-osteoporotic-fractures-in-premenopausal-women-and-men-50-years-old-with-systemic-lupus-erythematosus/