Session Information
Date: Tuesday, October 23, 2018
Title: Osteoporosis and Metabolic Bone Disease – Basic and Clinical Science Poster
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Identification of osteoporosis as a reason for vertebral fractures in patients with rheumatoid arthritis and non-inflammatory musculoskeletal diseases – A comparison between trabecular bone score (TBS) and bone mineral density (BMD)
Buehring B, Baraliakos X, Thomas J, Braun J. Rheumazentrum Ruhrgebiet, Herne, Germany.
Background/Purpose: Osteoporosis related fractures are common in patients with rheumatoid arthritis (RA). Measurement of bone mineral density (BMD) by dual energy X-ray absorptiometry (DXA) alone does not adequately predict fracture risk. Trabecular bone score (TBS) is a surrogate marker for trabecular microarchitecture which independently predicts fracture risk. In this study we assessed the prevalence of low BMD, low TBS and osteoporotic related vertebral fractures in patients with RA in comparison to controls with non-inflammatory musculoskeletal diseases.
Methods: In retrospective study design, we analyzed the data of all patients with available TBS and DXA data presenting to our hospital in the last 5 years. All diagnoses were made by rheumatologists. Comparisons between groups were made by Mann-Whitney-Test and Wilcoxon-Test where appropriate, after adjustment for age, cortisone intake and body mass index.
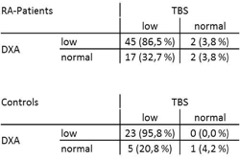
Results: There were 143 patients with RA (mean age 72.1±11.1 years, 72% female) and 106 controls (mean age 69.6±12.6 years, 74.5% female). Vertebral fractures were found in 36.4% (n=52) RA patients and in 22.6% (n=24) controls (p=0.02). Overall, there were no differences in the mean DXA BMD (for both, spine and hips) and the mean TBS values in all patients. On the other hand, there were statistically more RA patients with low BMD (n=102; 71.3%) and TBS scores (n=125; 87.4%) than controls (n=61; 57.5% and n=79; 74.5%, respectively, p=0.009). In addition, in patients with a vertebral fracture, a low TBS with a normal DXA was more frequently observed in both groups (numerically higher in RA than in controls), while low BMD with a normal TBS was rare (Table). This was not the case in patients without a vertebral fracture.
Conclusion: Low TBS in the setting of normal BMD was found more frequently in patients with vertebral fractures, especially in patients with RA, whereas the reverse is rare. This suggests TBS might prove to be a useful tool for identification of deteriorated bone microarchitecture and strength in patients with vertebral fracture with normal BMD.
Table: Prevalence of low and normal BMD and TBS results in patients with incident vertebral
fractures
To cite this abstract in AMA style:
Buehring B, Baraliakos X, Thomas J, Braun J. Identification of Osteoporosis As a Reason for Vertebral Fractures in Patients with Rheumatoid Arthritis and Non-Inflammatory Musculoskeletal Diseases – a Comparison between Trabecular Bone Score (TBS) and Bone Mineral Density (BMD) [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/identification-of-osteoporosis-as-a-reason-for-vertebral-fractures-in-patients-with-rheumatoid-arthritis-and-non-inflammatory-musculoskeletal-diseases-a-comparison-between-trabecular-bone-sc/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-osteoporosis-as-a-reason-for-vertebral-fractures-in-patients-with-rheumatoid-arthritis-and-non-inflammatory-musculoskeletal-diseases-a-comparison-between-trabecular-bone-sc/