Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Uveitis is the most common inflammatory eye disease and is frequently associated with secondary systemic autoimmune diseases (SSAID) excluding infection in 40-55% of cases. This analysis was undertaken to assess the diagnostic prevalence of patients of these disorders in patients with uveitis being evaluated by ophthalmology in a tertiary referral center.
Methods: Patients aged 18 years and older with uveitis, diagnosed and followed by ophthalmology from January 2013 to March 2018 were identified. By using the patient cohort explorer, an online visit processing tool, a search for diagnostic codes for uveitis (91 separate ICD-9 and ICD-10 codes) was performed. Individual searches for commonly associated SSAID were further done using ICD-9 and 10 codes to sub-categorize these patients. The search results were cross-referenced by running three additional data searches including medications administration, laboratory and imaging evaluation, and referral to rheumatology. Diagnostic prevalence was calculated and compared to historical data.
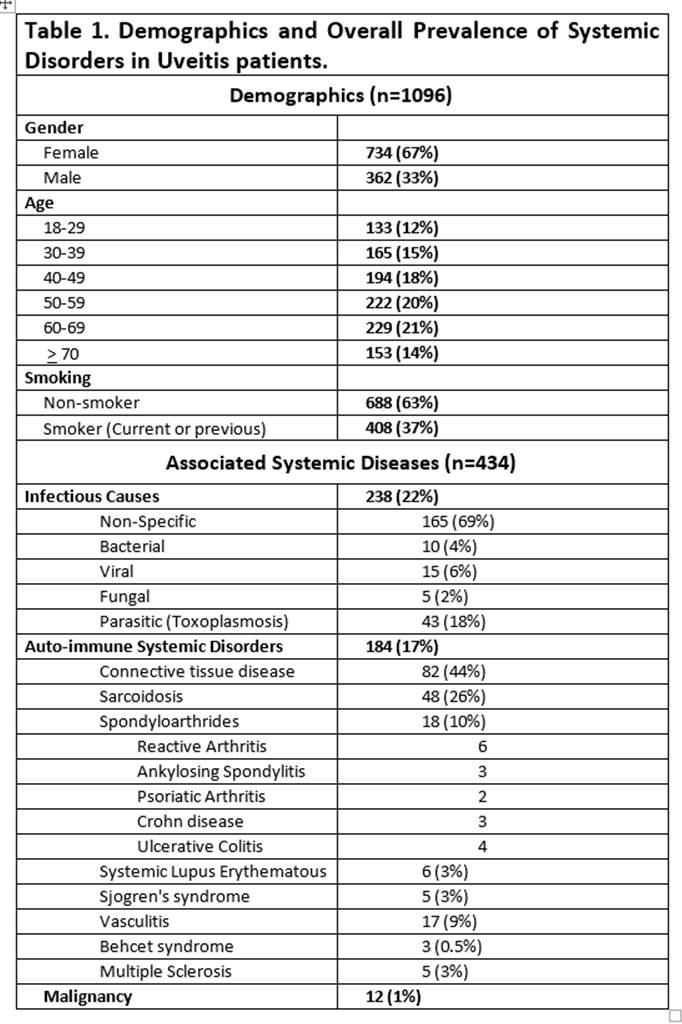
Results: There was a total of 1096 patient with uveitis. The majority of patients were female (67%). There was a high prevalence of smoking (37%) and the prevalence of uveitis increased with each decade of life. Only 17% of the cases had a concomitant diagnosis or evaluation for a SSAID, 22% had a diagnosis of an underlying infectious cause and only 1% due to malignancy. Table 1 shows the demographic data and relative frequency of prevalence in these disorders. Non-specific connective tissue disease was the most common diagnosis in SSAID, followed by sarcoidosis and vasculitis. Seronegative spondyloarthritides were only diagnosed in 18 patients (1.6%). HLA-B27 was only checked in 67 patients (6.1%) with 50% being positive.
Conclusion: Evaluation for and prevalence of systemic disease associated with uveitis was significantly lower (17%) than what was expected historically (40-55%). Even though this data is limited by the lack of individual review, the data obtained showed similar results through 4 different algorithmic searches. Smoking, a known risk factor for inflammation, was found at a higher prevalence than the general population, and there was an increase in the prevalence of uveitis with older age till 70 years. These data suggest that, despite overwhelming evidence, patients with uveitis may not be adequately evaluated for these systemic diseases. Strategies to improve education and perhaps targeted diagnostic algorithms may improve the detection of secondary systemic diseases.
References:
1. Rosenbaum JT. Uveitis. An internist’s view. Arch Internal Med 1989;149(5):1173-6.
2. Henderly DE, Genstler AJ, Smith RE et al. Changing patterns of uveitis. Am J Ophthalmol 1987;103(2):131-6.
3. Buitenhuis HJ, Meenken C, Brinkman CJ, et al. Uveitis and systemic disease. Br J Ophthalmol 1992;76(3):137-41.
To cite this abstract in AMA style:
Harrison N, Boddeda S, Kishore S, Majithia V. Missed Opportunity? Evaluation for Systemic Autoimmune Diseases in Patients with Uveitis May Not be Optimal: 5-Year Analysis of Patients Being Seen in a Tertiary Medical Center [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/missed-opportunity-evaluation-for-systemic-autoimmune-diseases-in-patients-with-uveitis-may-not-be-optimal-5-year-analysis-of-patients-being-seen-in-a-tertiary-medical-center/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/missed-opportunity-evaluation-for-systemic-autoimmune-diseases-in-patients-with-uveitis-may-not-be-optimal-5-year-analysis-of-patients-being-seen-in-a-tertiary-medical-center/