Session Information
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 9:00AM-11:00AM
Background/Purpose:
Most patients with RA receive oral glucocorticoids (GC) such as prednisone, despite concerns about safety. We sought to evaluate how primary care physicians (PCPs) use GC to treat RA patients co-managed by rheumatology, and whether PCP perceptions of GC side effects influences willingness to use GC for established RA patients.
Methods:
In 2017, we conducted an online, cross-sectional survey of American College of Physicians members, using its Internal Medicine Insider Research Panel. PCPs without subspecialty training spending ≥25% time in direct patient care were invited to participate. We developed a vignette featuring a hypothetical 62-year-old woman with RA co-managed by a rheumatologist, at increased risk for several GC side effects, who presents with severe RA flare. Respondents selected management options from a prepopulated list including laboratory tests, imaging studies, and treatments (GC, NSAIDs, and DMARDs). Participants willing to initiate oral GC were asked how long they would be willing to continue treatment.
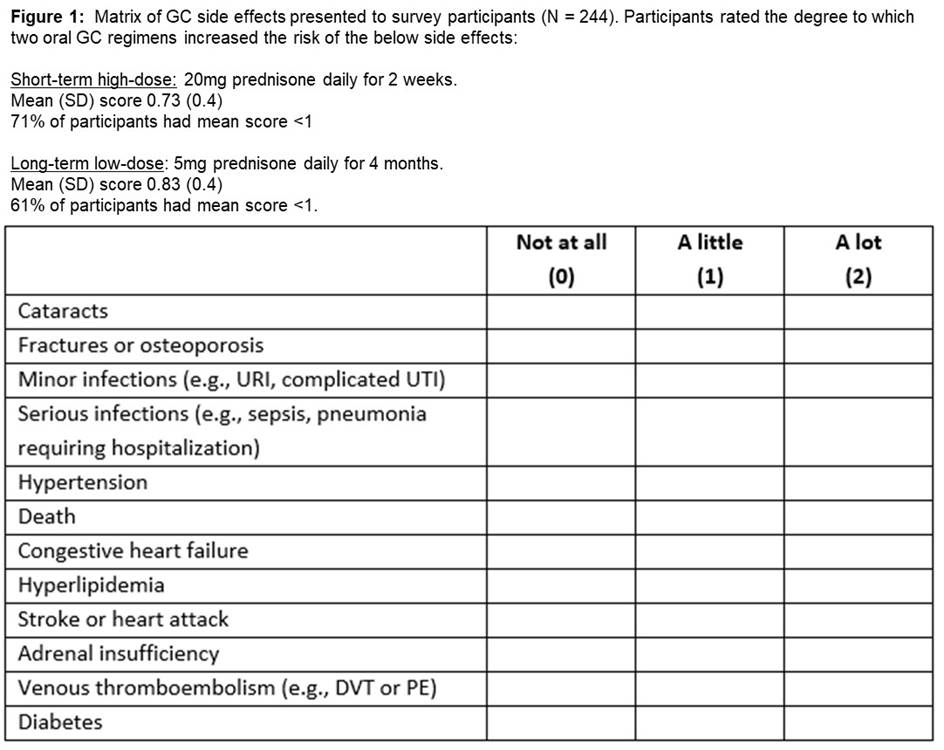
Participants rated the degree to which two different oral GC regimens increased risk of 11 GC side effects (Fig. 1). Response scores for each regimen were averaged; mean score <1 indicated a PCP thought side effects were unlikely with that regimen. We used multivariable linear regression adjusted for provider and practice characteristics to estimate the association between PCP concern about GC side effects and duration of GC prescribed.
Results:
244 of 557 eligible physicians (44%) completed the survey. Mean age was 51 years (SD 10.6), 35% were female, 74% in non-academic practice, and 51% practiced in a suburban area. In the 6 months prior to the survey, 58% had encountered a patient experiencing RA flare. Most reported patients in their panels had no significant difficulties affording medications or accessing a rheumatologist.
205 respondents (84%) were willing to prescribe oral GC for the hypothetical patient in the vignette. 164 (67%) would prescribe ≥20mg burst/taper of prednisone equivalent; 37 (15%) would prescribe Medrol Dosepak. 124 (51%) were willing to continue GC for ≥4 weeks; 53 (22%) were willing to continue for ≥6 weeks. Most PCPs perceived GC side effects as unlikely, regardless of regimen (Fig 1). PCP perception of GC side effects did not predict duration of GC prescribed (p=0.2 overall, 0.5 short-term high-dose, 0.2 long-term low-dose)
Conclusion:
In this national sample, 51% of PCPs were willing to prescribe ≥1 month of GC to an RA patient at high risk for GC side effects, despite their perception that their patients have good access to rheumatology care and RA medications. The duration of GC they were willing to prescribe was independent of concern about GC side effects. Poor communication between PCPs and rheumatologists, combined with PCP discomfort managing DMARDs, may contribute to GC overprescribing and thus avoidable side effects
To cite this abstract in AMA style:
Wallace B, Waljee A, Weissman A, Caverly T, Saini S. Overuse of Glucocorticoids in Rheumatoid Arthritis: A National Survey of Primary Care Physicians [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/overuse-of-glucocorticoids-in-rheumatoid-arthritis-a-national-survey-of-primary-care-physicians/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/overuse-of-glucocorticoids-in-rheumatoid-arthritis-a-national-survey-of-primary-care-physicians/