Session Information
Date: Tuesday, October 23, 2018
Title: Epidemiology and Public Health Poster III: SLE, SSc, APS, PsA, and Other Rheumatic Diseases
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Therapeutic plasma exchange (TPE) or plasmapheresis is a process in which plasma containing components, including autoantibodies and immune complexes, can be removed from the circulation. The ability to do so makes TPE an option for the treatment of immune-mediated diseases, including many rheumatologic diseases (RDs). In RDs, TPE can help to rapidly decrease the circulating levels of antibodies, while buying time for the immunosuppressive medications to take effect. The aim of our study was to compare the utilization of plasmapheresis among patients with select RDs and to assess the yearly trends in terms of Annual Percentage Change (APC).
Methods:
We used National (Nationwide) Inpatient Sample database from the years 2000-2014 to identify inpatients ≥18 years with the diagnosis of autoimmune RDs based on ICD-9 codes. We compared the utilization of therapeutic plasmapheresis in RDs with that in Goodpasture’s syndrome (a rare autoimmune and a prototypical renal disease in which plasmapheresis remains the treatment of choice). Anti-phospholipid syndrome was not used in the analysis due to unavailability of discrete ICD-9 code for the condition. Joinpoint regression analysis software was used to calculate the APC and to determine if the annual change in trend was statistically significant or not.
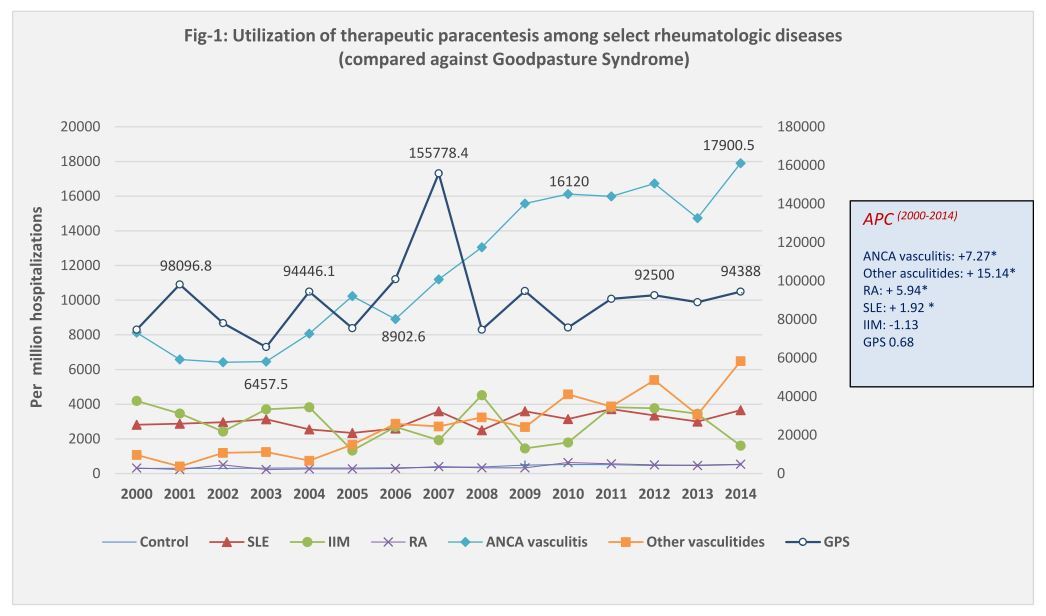
Results:
Among hospitalized adults, the utilization of TPE was much higher in Goodpasture’s syndrome compared to any one of the studied RDs. However, a significantly increasing trend was noted among RDs, most notably the anti-neutrophil cytoplasmic antibody (ANCA)-vasculitis and other Vasculitides. The utilization of TPE in Goodpasture’s syndome was ~ 74,000 per million hospitalizations on 2000 compared to ~ 94,000 in 2014. Among various RDs, the highest utilization was noted in ANCA associated vasculitis, and the rate doubled from 8000 per million hospitalizations on 2000 to over 16,000 per million on 2014, with an annual increase of 7.27%. Significant increase in trend was also noted among hospitalizations with other Vasculitides (APC of 15.14) (Figure 1).
Conclusion:
The steady increase in the utilization of TPE for patients with RDs, mostly the ANCA and non-ANCA associated Vasculitides may be reflective of the mounting data suggesting improved outcomes and decreased progression to end-stage renal disease when TPE is used in addition to immunosuppression. While some case reports and controlled trials have demonstrated treatment benefit from plasmapheresis in patients with SLE and IIM, others have found no improvement in clinical course. While plasmapheresis is relatively safe (mortality rate of ~0.05%), the most common adverse reactions are hypocalcaemia, hypovolemia and rarely anaphylactic reaction. Further studies need to be performed to determine the safety and cost-effectiveness of plasmapheresis as a treatment option for RDs.
To cite this abstract in AMA style:
Dhital R, Lynn T, Sharma P, Basnet S, Paudel P, Pyakurel S, Poudel D. The Trend of Utilization of Therapeutic Plasmapheresis Among Select Rheumatologic Diseases [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/the-trend-of-utilization-of-therapeutic-plasmapheresis-among-select-rheumatologic-diseases/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-trend-of-utilization-of-therapeutic-plasmapheresis-among-select-rheumatologic-diseases/