Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The epidemiology of pediatric vasculitis is poorly described. Two studies in the 1990s described the frequency in pediatric rheumatology centers in the United States and Canada (1.2-2.4% of rheumatologic diagnoses). Subsequently, consensus classification criteria for pediatric vasculitis were developed, yet disease patterns have not been reassessed. Although many immunomodulatory regimens are used, practice patterns for treatment of pediatric vasculitis are not known. Recently, the Childhood Arthritis and Rheumatology Research Alliance developed a registry of children treated at pediatric rheumatology centers in the United States (CARRAnet). The purpose of this study was to delineate the distribution and treatment of vasculitides within the first 24 months of CARRAnet.
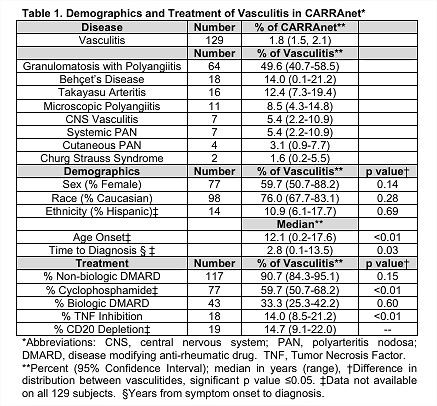
Methods: This is a retrospective observational cohort study using CARRAnet. 55 centers submitted data on patients with defined rheumatologic disease (vasculitis, 35 centers) (May 2010-May, 2012). Not all patients with these diagnoses at each study site were included. Demographic, diagnostic evaluation, disease manifestation, and treatment data were collected using standardized forms and entered into an electronic database. This cohort includes children with vasculitis: granulomatosis with polyangiitis (GPA); Beh�et’s disease (BD); Takayasu arteritis (TAK); microscopic polyangiitis (MPA); central nervous system vasculitis (CNSV); systemic polyarteritis nodosa (PAN); cutaneous PAN; Churg-Strauss syndrome (CSS).
Results: 129 children, 1.8% of the registry, had vasculitis (Table 1). The median age of onset was 12.1 years; the median time to diagnosis was 2.8 years. There was a significant difference in the distribution of the age at onset (p<0.01), but not in the distribution of sex, race, or ethnicity (p=0.14, p=0.28, p=0.68), between vasculitides. Most children were treated with glucocorticoids (96%) and a non-biologic disease modifying anti-rheumatic drug (DMARD) (91%); 60% were treated with cyclophosphamide. 33% were treated with a biologic DMARD: tumor-necrosis factor inhibition (14%); CD20-depletion (15%).
Conclusion: While the frequency of vasculitis in CARRAnet is similar to that in earlier clinic-based registries, the distribution of diagnoses differs in that a greater percentage of children had GPA and TAK and a smaller percentage MPA. Compared to a recent pediatric GPA cohort, despite the increased use of CD20 depletion (15 vs. 1.5%), children were not spared exposure to cyclophosphamide (75 vs. 83%). Among pediatric rheumatology centers, treatment regimens for vasculitis vary considerably. This study demonstrates the usefulness of CARRAnet to study pediatric rheumatic conditions, especially rare vasculitides. Expanded enrollment of the cohort, and follow-up of cases, will provide important observational data not obtainable by single-center studies.
Disclosure:
M. A. Lerman,
None;
P. A. Merkel,
None;
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/distribution-of-vasculitides-in-childhood-arthritis-and-rheumatology-research-alliance-affiliated-pediatric-rheumatology-centers-in-the-united-states/