Session Information
Date: Monday, October 22, 2018
Title: 4M103 ACR Abstract: Pain Mechanisms–Basic & Clinical Science (1917–1922)
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Experts have implicated physician prescribing rates as a contributing factor to the opioid crisis. However, little is known about heterogeneity in these patterns and its effects on chronic opioid use. Our objectives were to: 1) identify the extent to which US physicians varied in baseline opioid prescribing rates, and 2) determine the implications of physicians’ baseline opioid prescribing rates on future probability of chronic opioid use among rheumatoid arthritis (RA) patients.
Methods: Data were obtained from the Corrona Rheumatoid Arthritis Registry. To ensure robust baseline opioid prescribing information, physicians were included in the analyses only if they contributed ≥10 RA patients within the first 12 months of participation in the registry. RA patients were included if they: 1) were patients of the included physicians, 2) had ≥12 months follow-up, and 3) were not prevalent opioid users at study entry. Baseline opioid prescribing rates were calculated using data from RA patients seen within the first 12 months after a physician began participating in the registry, dividing the number of patients reporting opioid use by the number of patients seen during that year. The baseline opioid prescribing rate was then assessed as the exposure of interest in models that predicted chronic opioid use in patients seen subsequent to the baseline 12 month period. Generalized linear mixed models, controlling for relevant patient, physician and site characteristics, were used to assess the relationship between baseline prescribing rates and future chronic opioid use. Subgroup analyses were done to examine heterogeneity across the following clinical characteristics: 1) disease activity, defined by Clinical Disease Activity Index (CDAI) score ≤10 vs. >10; 2) pain intensity (≤40, >40-60, >60 out of 100); and 3) antidepressant use (yes/no). Interaction terms were used to assess the statistical significance of differences between subgroups.
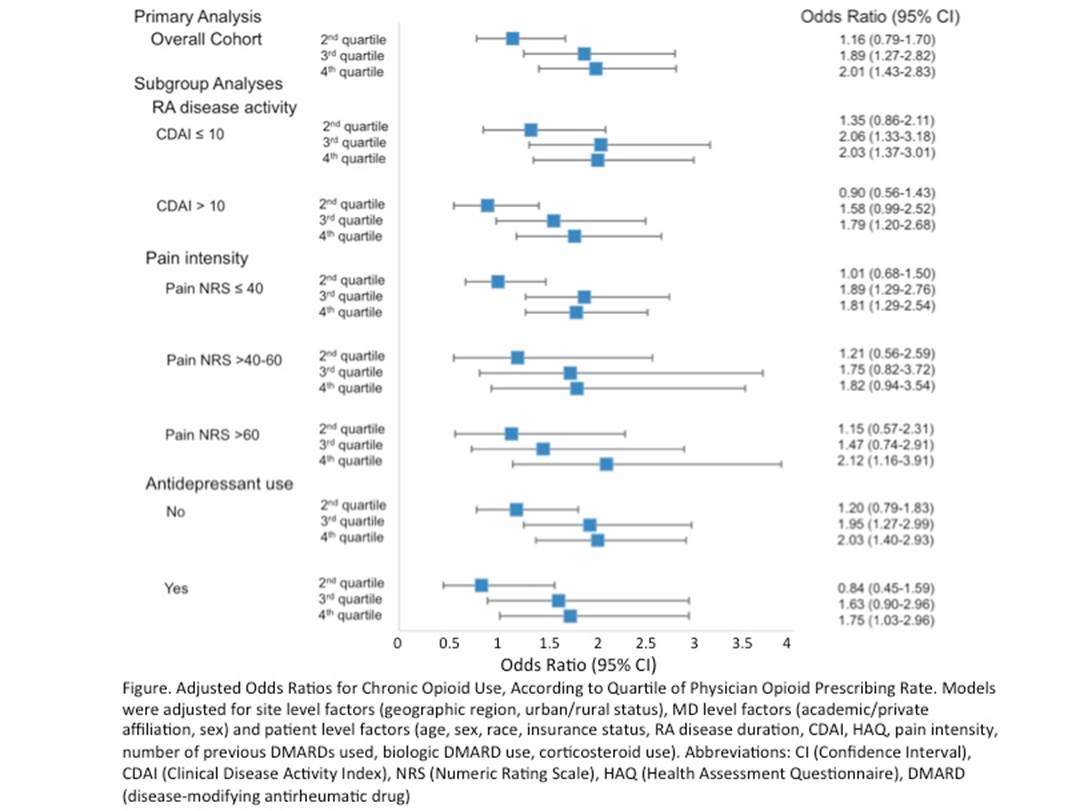
Results: Among the 148 physicians in the initial cohort, baseline opioid prescribing rates varied from 0-70%, with a median of 27% and interquartile range of 18-37%. Among the 9337 RA patients included in the period after the baseline 12 months, physician opioid prescribing rates during the baseline period were significantly associated with risk for chronic opioid use (ref: lowest quartile; 2nd quartile: OR 1.16, 95% CI 0.79-1.70, 3rd quartile: 1.89, 95% CI 1.27-2.82, 4th quartile: OR 2.01; 95% CI 1.43-2.83) (Figure). No statistically significant differences were noted between subgroups.
Conclusion: Rates of baseline opioid prescribing varied widely. A physician’s baseline opioid prescribing rate was a strong predictor of whether a patient would become a chronic opioid user in the future, even after controlling for patient characteristics.
To cite this abstract in AMA style:
Lee YC, Lu B, Guan H, Greenberg J, Kremer J, Solomon D. Physician Opioid Prescribing Patterns and Risk for Chronic Opioid Use Among Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/physician-opioid-prescribing-patterns-and-risk-for-chronic-opioid-use-among-rheumatoid-arthritis-patients/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/physician-opioid-prescribing-patterns-and-risk-for-chronic-opioid-use-among-rheumatoid-arthritis-patients/