Session Information
Date: Monday, October 22, 2018
Title: 4M094 ACR/ARHP Abstract: Health Services Research I: Focus on Big Data (1887–1892)
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose:
The Department of Veterans Affairs (VA) operates the largest integrated health care system in the U.S. The proportion of Veterans with RA who receive high quality care within VA is unknown. Our objective was to quantify the proportions of Veterans with RA nationwide who were prescribed a DMARD in 2016, and identify Veteran- and system-level correlates of DMARD receipt.
Methods: Cross-sectional study of national VA data examining DMARD receipt in 2016 among Veterans with RA who received care within VA. RA and DMARD use were identified using HEDIS technical specifications (including ICD-9 and ICD-10 diagnosis codes) for 2016. Veteran-level (age, gender, race, poverty level, comorbidity score, substance use disorder, post-traumatic stress disorder (PTSD)) and system-level (health care region, facility complexity, rheumatologist shortage area) correlates were examined using bivariate and multivariate logistic regression.
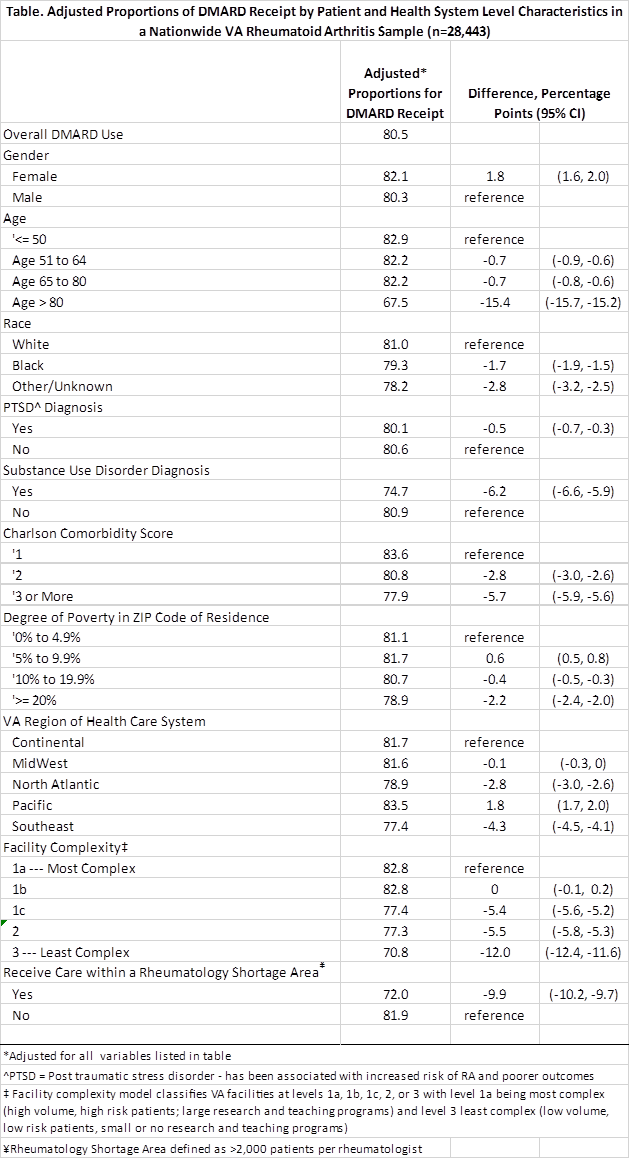
Results: 28,443 unique Veterans with RA were identified in the VA health care system:13% were female, 77% white, and 55% age 65-80. Nearly half had a Charlson comorbidity ≥3, 12% had PTSD and 6% substance use disorder. Overall, 80.5% received a DMARD in 2016. DMARD receipt was similar by race and sex, but we found significant variation based on older age, presence of substance use disorder, and higher Charlson comorbidity score (see Table). We also found significant geographic and system-level effects, including lower DMARD use in less complex facilities and those in rheumatology shortage areas (Table).
Conclusion: In 2016, quality of care among Veterans with RA (as measured by the proportion receiving a DMARD) who receive care within VA was equal to or higher than rates for those receiving care in Medicare health maintenance (HMO) or preferred-provider organization (PPO) settings (76.8% and 77.8%, respectively). It far exceeded rates reported among Medicare beneficiaries a decade ago. However, Veterans with multimorbidity and older age were less likely to receive a DMARD as were those living in the North Atlantic and Southeast. Specialty rheumatology care plays a vital role in quality of care. Future work should examine approaches to increase the reach of this specialty care to all VA patients and aim to reduce Veteran and system level variation.
To cite this abstract in AMA style:
Barton J, Herrndorf A, Schmajuk G, Matsumoto RA, Ganzini L, Carlson K. Patient and Health System Characteristics Associated with Receipt of Disease Modifying Anti-Rheumatic Drugs in a National VA Sample [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/patient-and-health-system-characteristics-associated-with-receipt-of-disease-modifying-anti-rheumatic-drugs-in-a-national-va-sample/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/patient-and-health-system-characteristics-associated-with-receipt-of-disease-modifying-anti-rheumatic-drugs-in-a-national-va-sample/