Session Information
Date: Monday, October 22, 2018
Title: 4M083 ACR Abstract: Healthcare Disparities in Rheumatology (1840–1845)
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Population-based SLE mortality studies have depended on administrative data from vital statistics records to identify cases. However, a high proportion of SLE deaths have no SLE code. We studied mortality trends from a population-based registry that overcame many of these limitations.
Methods: The Georgia Lupus Registry is a CDC funded population-based registry of validated SLE patients in Atlanta, Georgia from 2002-04. The state privacy exemption for surveillance allowed health care providers and facilities to provide access to protected health information without written patient consent, allowing for validation of diagnoses on a population level using ≥4 ACR criteria or 3 ACR criteria with a final diagnosis of SLE by a board-certified rheumatologist. All incident and prevalent SLE cases were matched to the National Death Index, which contains information for all deaths in the U.S. as derived from information on death certificates and provided by local vital records offices, through 2016. Cumulative mortality survival analysis and standardized mortality rates (SMR) were analyzed.
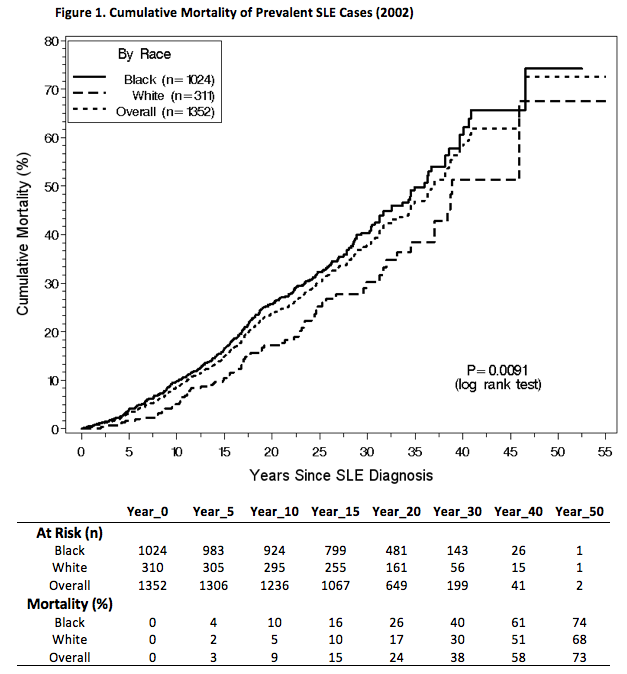
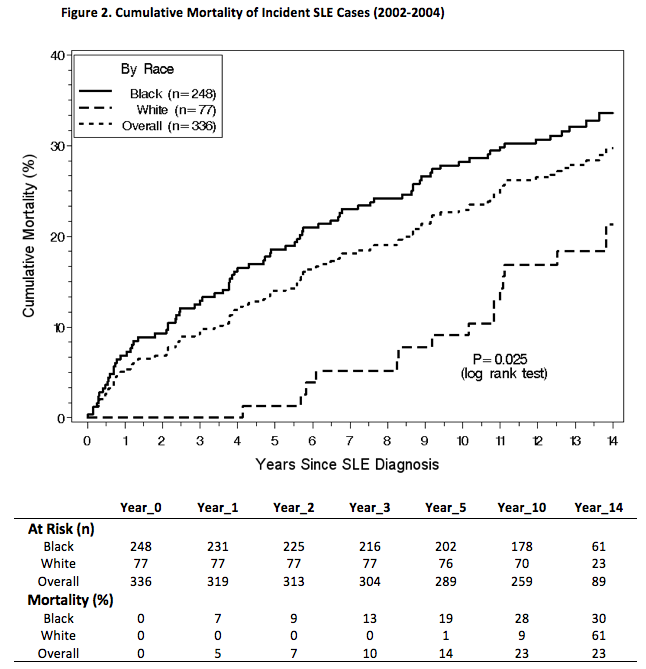
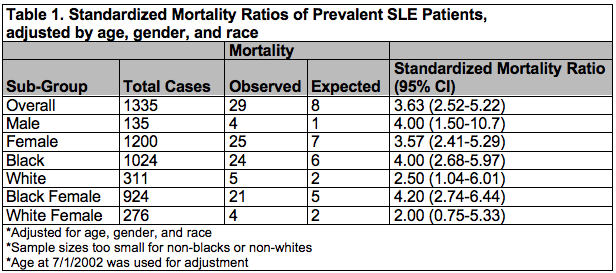
Results: Of 336 incident SLE patients in 2002-04, 86.9% were female, 73.8% black and 22.9% white, and mean age of 40.6 years at SLE diagnosis. Of 1353 prevalent SLE patients in 2002, 89.9% were female, 75.7% black and 23% white, and mean age of 34.6 years at SLE diagnosis. There were 97 deaths through 2016. Blacks had significantly greater cumulative mortality than whites (Figs. 1 and 2) and were younger at death for both incident (51.8±17.5 vs. 64.4 ± 18.9, P=0.013) and prevalent (52.3 ± 15.9 vs. 65.0 ± 16.3, P=<0.0001) cases. Whites had a marked lower mortality after diagnosis compared with blacks; For incident cases, whites did not die until 5 years after SLE diagnosis, whereas blacks had significant and persistent higher mortality from the start. There were no significant differences by gender. SMR’s were calculated for prevalent patients (Table 1).
Conclusion: Despite increasing awareness and advancements in treatment, mortality in SLE continue to remain high and disparate across combined gender and race groups with the highest standardized mortality ratio in black females. Defining and addressing reversible mortality factors must be high priorities in mitigating racial disparities and improving overall outcomes in SLE.
To cite this abstract in AMA style:
Lim SS, Helmick CG, Bao G, Gordon C, Hootman JM, Drenkard C. Racial Disparities and Accelerated SLE Mortality from a Population-Based Registry: The Georgia Lupus Registry [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/racial-disparities-and-accelerated-sle-mortality-from-a-population-based-registry-the-georgia-lupus-registry/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/racial-disparities-and-accelerated-sle-mortality-from-a-population-based-registry-the-georgia-lupus-registry/