Session Information
Date: Monday, October 22, 2018
Title: Spondyloarthritis Including Psoriatic Arthritis – Clinical Poster II: Clinical/Epidemiology Studies
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
The severe consequences of osteoporosis in the general population are well outlined. In axial spondyloarthropathy (axSpA), osteoproliferation of the spine means posterioanterior (PA) dual-energy x-ray absorptiometry (DXA) can’t discriminate between new bone formation and vertebral body, potentially overestimating BMD. To understand the impact of low BMD in axSpA, we need an accurate and reproducible method of assessment. Lateral DXA of the spine avoids spinal osteoproliferation and is an attractive option. The aim of this study is to compare lateral DXA of the lumbar spine with PA DXA, and determine patient variables that render conventional DXA unreliable.
Methods:
Patients fulfilling modified New York (mNY) or Assessment of Spondyloarthritis International Society (ASAS) criteria were consecutively recruited from rheumatology clinics in this twin-centre cross-sectional study. A detailed assessment of patients included demographics, clinical exam, laboratory assessment and validated measures of disease severity (BASDAI, ASDAS-CRP, BASMI, mSASSS). BMD of the spine was assessed using DXA in the lateral and PA projections. BMD of the hip was assessed in the conventional manner. R software was used for statistical analysis.
Results:
One hundred and ten patients were assessed, 100 of whom had paired AP and lateral DXAs: 76% (n=84) male, 92% Caucasian, 81% mNY criteria. Median (IQR) age was 52 (17) years, disease duration 23.5 (20) years, delay to diagnosis 7 (12) years, body mass index (BMI) 27.6 (6.3) kg/m2, BASDAI 3.9 (2.1-5.6), BASMI 4.1 (2.8-5.8), ASDAS-CRP 2.2 (1.5-3), mSASSS 8.5 (2-36).
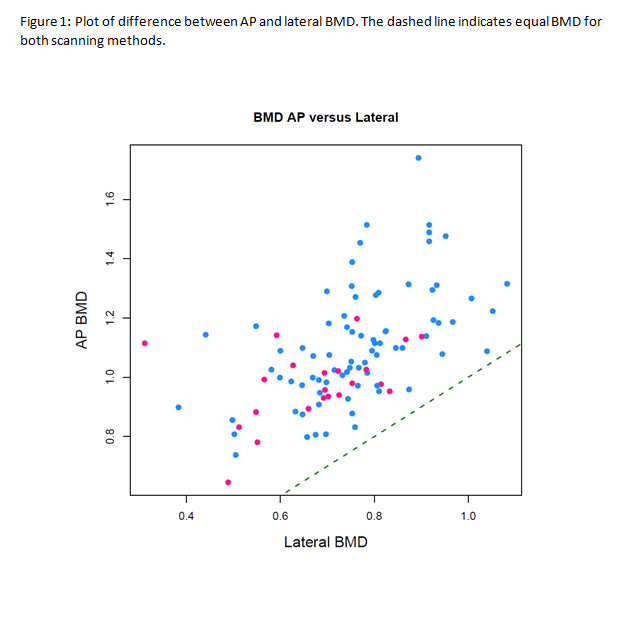
Lateral spine BMD is significantly lower than PA BMD (see figure 1), with a mean difference between AP and lateral lumbar spine DXA of 0.337 g/cm2 (95% CI 0.3-0.37), and detects more cases of both osteopenia (27% versus 17%) and osteoporosis (16% versus 2%) at the spine (p<0.01). The prevalence of osteopenia at the hip is 25% and osteoporosis is 1%. When combined with hip DXA to assess for low BMD at any site, using lateral DXA characterises 52% of the cohort as having low BMD, in comparison to 36% when AP DXA is used (p<0.01).
The following variables correlate with a larger difference between the measurement of AP and lateral DXA: BASMI (r=0.54), disease duration (r=0.37), BMI (r=0.32), mSASSS (r=0.52).
In multiple regression analysis, a model with disease duration, BMI, BASMI and shorter time to diagnosis predicts a greater difference between AP and lateral BMD (p<0.05).
Conclusion:
Lateral DXA detects more cases of low BMD than PA DXA, particularly in patients with higher BASMI and BMI and longer disease duration. Continuing to rely on AP DXA will miss a significant number of axSpA patients with low BMD. Lateral DXA is a practical and feasible tool suitable for use in clinical practice and should be considered as an alternative to PA when measuring BMD in the lumbar spine.
To cite this abstract in AMA style:
Fitzgerald G, Wyse J, Anachebe T, Mullan R, Kane D, McCarroll K, O' Shea F. Lateral DXA More Effective in Detecting Osteoporosis Than Conventional DXA in Axial Spondyloarthropathy [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/lateral-dxa-more-effective-in-detecting-osteoporosis-than-conventional-dxa-in-axial-spondyloarthropathy/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lateral-dxa-more-effective-in-detecting-osteoporosis-than-conventional-dxa-in-axial-spondyloarthropathy/