Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Sjögrenfs syndrome (SS)-associated neuropathy manifests as various forms of neuropathy, including sensory ataxic neuropathy (SAN). Dorsal root ganglionitis, pathologically defined as the lymphocytic infiltration of the dorsal root ganglion (DRG), causes SAN. This study aimed to determine whether 3-Tesla magnetic resonance neurography (3T-MRN) is useful for detecting abnormalities of DRGs, and making diagnoses in patients with SS-SAN.
Methods: We conducted a retrospective chart review from 2015 to 2017 and enrolled 3 patients with SS-SAN fulfilling American–European Consensus Group classification criteria. We evaluated with a 3T MRI scanner and used the coronal short-tau inversion recovery (STIR) technique because of its advantages in depicting a symmetric normal hyperintensity of DRGs and nerves. On measuring a pair of DRGs, regions of interest (ROI) were manually drawn by using ImageJ (http://rsb.info.nih.gov/ij/). The area, median SI, and transverse diameter of each DRGs were measured and compared with those of the corresponding proximal nerve roots. The SI ratio (SI within a DRG/SI within a proximal nerve root) and diameter ratio (transverse diameter of a DRG/width at the middle point of a proximal nerve root) were subsequently calculated. For each nerve root level, data from SS patients were compared with those of age- and sex-matched non-neuropathy controls (20 DRGs from 10 cases). All statistical analyses were performed with EZR, a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria). The Mann–Whitney U test was applied for the statistical analysis.
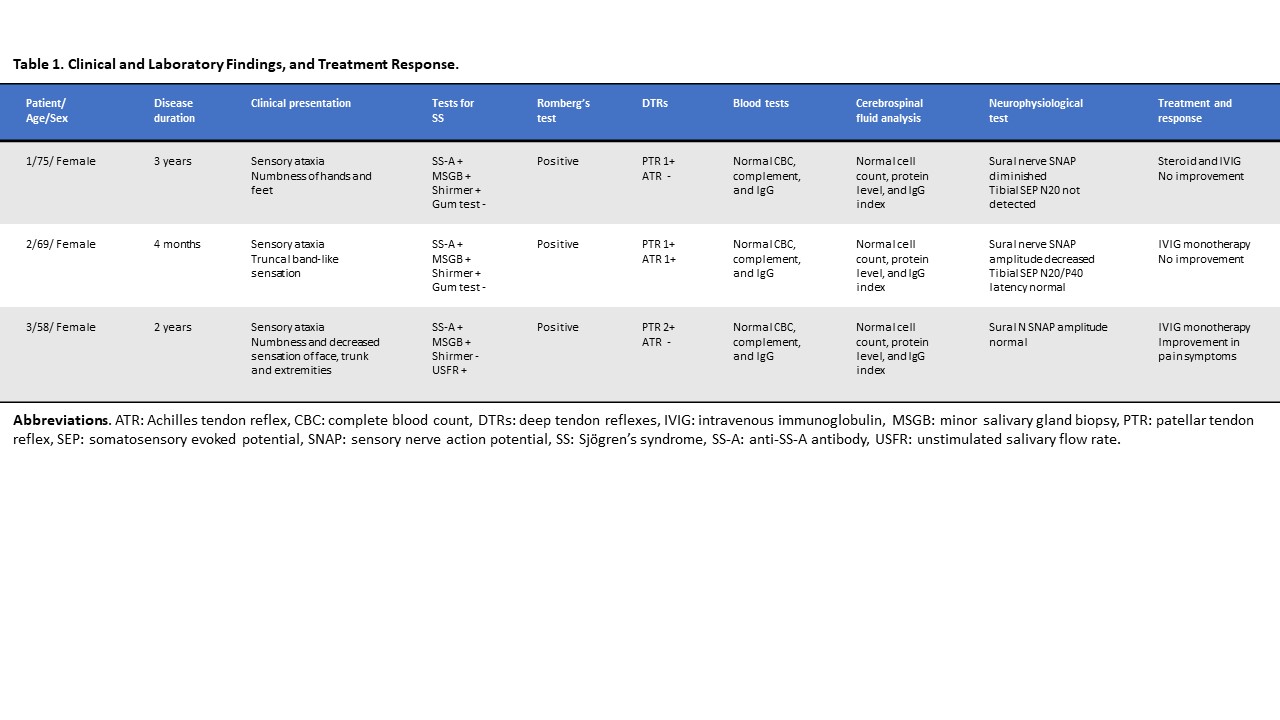
Results: Table 1 summarizes the clinical data of the 3 patients. These SS-SAN patients presented with sensory ataxia with positive Rombergfs test and also had various painful symptoms. All 3 patients showed normal motor strength. Compared with the control data, all DRGs in SS patients were numerically smaller and had a lower SI through the L2-S1 level. Moreover, the area, diameter ratio, and SI ratio were significantly reduced in L3-L4 DRGs (Table 2).
Conclusion: We revealed that the DRGs in patients with SS-SAN were atrophic and showed a decreased SI than those in the controls. We suggest the visualization of DRGs by 3T-MRN as a potentially useful imaging biomarker for the clinical diagnosis, as well as the assessment of pathophysiological mechanisms. DRG atrophy and decreased signal intensity may reflect the sensory neuronal loss caused by chronic lymphocytic inflammation in DRGs.
To cite this abstract in AMA style:
Yoshida T, Sueyoshi T, Kinjo M, Suwazono S, Nodera H. Visualization of Dorsal Root Ganglionitis with Three-Tesla Magnetic Resonance Neurography in Sensory Ataxic Neuropathy Associated with Sjögren’s Syndrome [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/visualization-of-dorsal-root-ganglionitis-with-three-tesla-magnetic-resonance-neurography-in-sensory-ataxic-neuropathy-associated-with-sjogrens-syndrome/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/visualization-of-dorsal-root-ganglionitis-with-three-tesla-magnetic-resonance-neurography-in-sensory-ataxic-neuropathy-associated-with-sjogrens-syndrome/