Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Laboratory testing comprises the highest volume procedure in medicine and is therefore an important target for improving healthcare spending and efficiency. Unnecessary testing both increases healthcare costs and results in higher false positive rates with associated costly downstream testing and procedures. Additionally, unnecessary testing increases the patient burden and may increase the probability of an adverse health event.
This study aimed to examine the utilization patterns, appropriateness, and associated cost of rheumatologic tests ordered for patients referred to a university rheumatology clinic. A secondary aim of this study was to determine whether demographic factors such as patient sex, reason for referral, and referring practice population size were predictive of inappropriate testing.
Methods:
This study consisted of a chart audit of consecutive referrals to three rheumatologists at an academic university rheumatology clinic over one year. All new referrals that had proper documentation, were not transfers of care, and did not have previously established diagnoses were considered. Of referrals that met inclusion criteria (n=631), 398 accepted and 233 rejected referrals were reviewed. Ordering of specific tests (ANA, ENA, anti-dsDNA, RF, and complement levels) and their appropriateness based on clinical presentation were extracted from medical charts. Lab tests ordered within 2 years prior to referral were collected for accepted referrals. Additionally, the reason for referral, diagnosis (accepted referrals), reason for rejection (rejected referrals), patient age and sex, and the population size of the referring practice was collected to identify potential predictors of inappropriate testing.
Results:
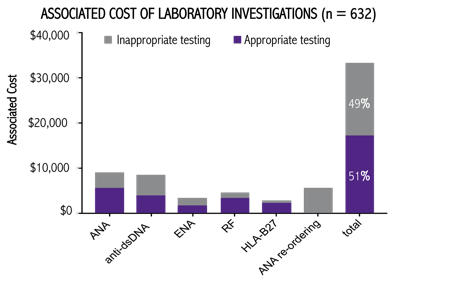
The number one reason for referral in accepted referrals and rejected referrals was seronegative spondyloarthropathy and fibromyalgia respectively. Of the referrals reviewed (n=631), 41% had at least one instance of inappropriate testing. ANA was most frequently ordered inappropriately, with 20% of all referrals having ANA testing with no clinical indication. Additionally, 56% of ANA testing in accepted referrals was repeated testing. Family physicians and nurse practitioners were significantly more likely to order inappropriate tests than specialists (p = 0.007). Chi-squared testing found patient age (p=0.445), gender (p=0.051), and population size (p=0.855) were not predictive of inappropriate testing.
Conclusion:
The results of this study showed a significant problem with inappropriate testing in referrals made to this institution. Cost estimation of inappropriate testing identified a potential cost reduction of 49%. Future research should focus both on implementing existing guidelines, and on creating interventions tailored to family medicine practice to produce the greatest reduction in cost.
To cite this abstract in AMA style:
Barrett S, Ahrari A, Rohekar S, Basharat P, Pope JE. An Evaluation of Utilization Patterns and Appropriateness of Laboratory Tests Among New Referrals to Rheumatologists: Choosing Unwisely! [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/an-evaluation-of-utilization-patterns-and-appropriateness-of-laboratory-tests-among-new-referrals-to-rheumatologists-choosing-unwisely/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-evaluation-of-utilization-patterns-and-appropriateness-of-laboratory-tests-among-new-referrals-to-rheumatologists-choosing-unwisely/