Session Information
Session Type: ACR/ARHP Combined Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Prior research has focused on factors important to clinicians in decisions about withdrawing JIA therapy. Based on recent interviews with patients and caregivers about stopping JIA therapy, we conducted an online survey to study the trade-offs patients and caregivers consider when deciding to stop treatments.
Methods: From June 2017 to February 2018, we conducted an anonymous online survey in English and Spanish using REDCap software. We recruited volunteer participants via social media, email, and flyers in pediatric rheumatology clinics in the US and Canada. Eligible participants were (1) adolescents with JIA (13-17y), (2) adults with JIA (≥18y), or (3) caregivers of children with JIA. Survey questions focused on factors that might influence decisions about stopping JIA treatment. Questions were based on findings from prior interviews and refined via pilot testing. We analyzed responses using descriptive statistics.
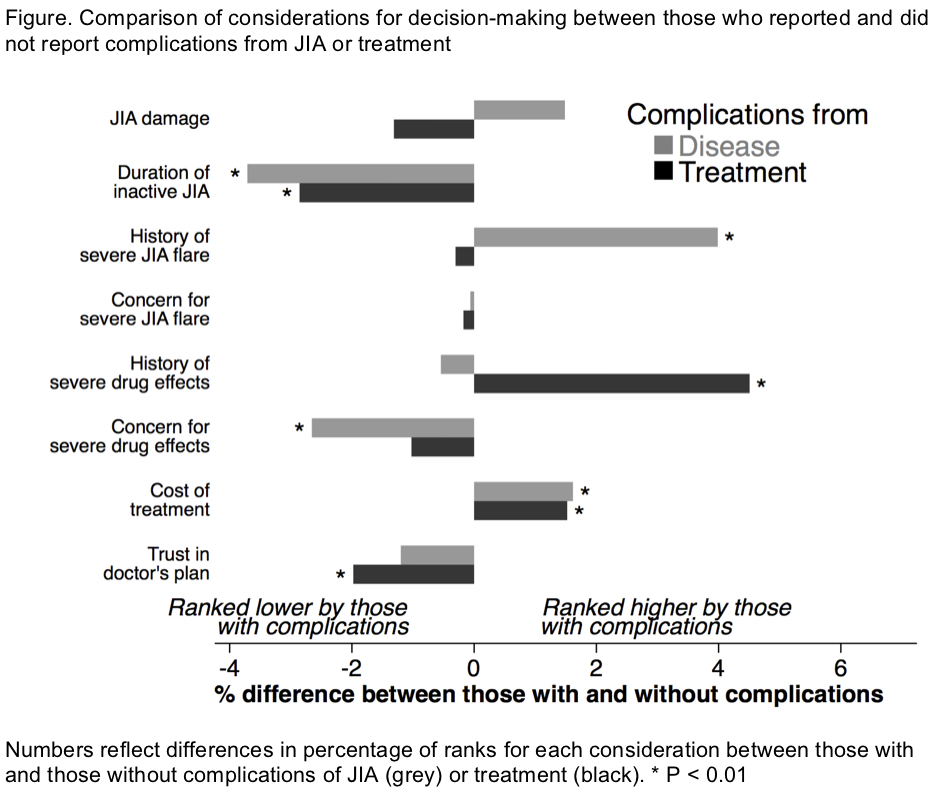
Results: 1456 individuals opened the survey and 839 (58%) completed it, including 782 eligible participants (40 adolescents, 120 young adults, and 622 caregivers).A majority of the participants were from the US, had a history of severe JIA flares, and used systemic anti-rheumatic medicines. Overall, adult patients were more likely than caregivers or adolescents to report having more severe disease and more complications from JIA and treatment. Among all groups, damage from JIA was the most highly ranked consideration in deciding whether to stop treatment (Table). Those with prior disease complications (e.g., severe flare, disability) were more likely to prioritize risk of flares in decision-making and generally less concerned about future drug effects (Figure). In contrast, those with prior treatment complications were more likely to prioritize risk of drug side effects (Figure). Trust in physicians was especially important for caregivers and adolescents (Table). Those reporting greater trust in physicians were more willing to accept physicians’ recommendations to continue or stop treatment (P<0.01).
Conclusion: Among survey respondents, JIA-related damage was the top consideration in deciding whether to stop treatments for well-controlled JIA. Past complications from JIA or from treatment influenced the ranking of other considerations. Greater trust in physicians increased willingness to accept physicians’ recommendations. These findings can help inform shared decision-making when considering whether to stop medicines for well-controlled JIA.
To cite this abstract in AMA style:
Horton DB, Salas J, Wec A, Beukelman T, Boneparth A, Guzman J, Haverkamp K, Kohlheim M, Mannion ML, Moorthy N, Stringer E, Tucker L, Ringold S, Rosenthal M. Stopping Medicines for Inactive Juvenile Idiopathic Arthritis: What Do Patients and Families Consider? [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/stopping-medicines-for-inactive-juvenile-idiopathic-arthritis-what-do-patients-and-families-consider/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/stopping-medicines-for-inactive-juvenile-idiopathic-arthritis-what-do-patients-and-families-consider/
