Session Information
Date: Sunday, October 21, 2018
Title: 3S102 ACR Abstract: Epidemiology & Pub Health I: Morbidity & Mortality (940–945)
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: RA is associated with increased total, cardiovascular, and respiratory mortality compared to the general population. This excess RA mortality may be mediated through lifestyle, clinical, or RA-specific factors occurring after diagnosis. Casual inference methods, such as marginal structural models, can adjust for both confounders as well as mediators on the causal pathway between RA diagnosis and mortality. We aimed to decipher the mechanism through which RA increases total and cause-specific mortality accounting for potential mediators after RA diagnosis using causal inference methods.
Methods: We used a prospective cohort study, the Nurses’ Health Study (n=121,700), to investigate RA and mortality, accounting for lifestyle/clinical covariates before/after RA diagnosis. We identified incident RA meeting ACR criteria during follow-up. We matched each RA case to 10 comparators by age and year at RA diagnosis (index date). We considered lifestyle/clinical factors assessed by biennial surveys as baseline confounders (before index date) or mediators (after index date). Lifestyle factors included smoking, BMI, diet, and physical activity. We used the validated Multimorbidity Weighted Index, composed of 64 prevalent/serious health conditions (interstitial lung disease [ILD] was unmeasured). We used inverse probability weights to adjust for the confounding/mediating effects of covariates on mortality risk for RA vs. comparators. We compared RA effect estimates for mortality in models composed of baseline confounders and time-updated mediators.
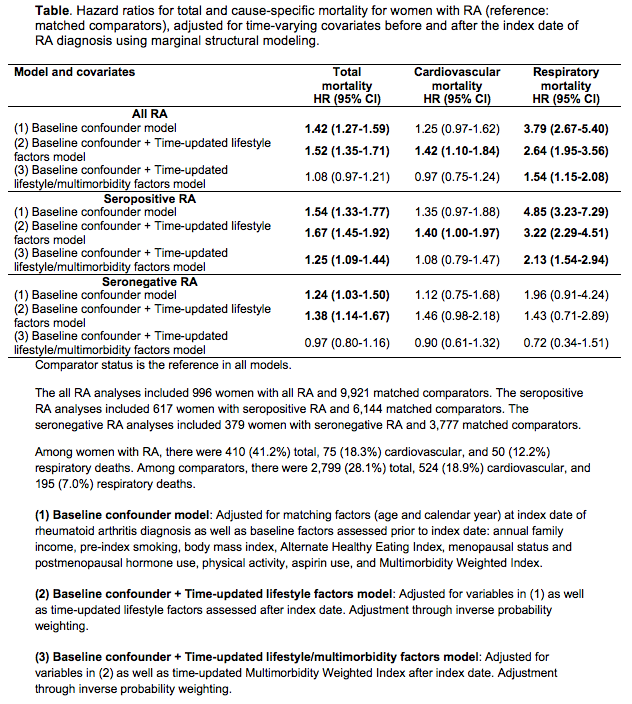
Results: At index date, mean age was 60.1 years (SD 10.2). Among 996 women with incident RA, 410 (41.2%) died during mean follow-up of 19.8 years (SD 9.1). Among 9,921 matched comparators, 2,789 (28.1%) died during mean follow-up of 19.5 years (SD 9.7). Adjusting for baseline factors and time-updated lifestyle factors after index date, RA was associated with excess total (HR 1.52, 95%CI 1.35-1.71), cardiovascular (HR 1.42, 95%CI 1.10-1.84), and respiratory (HR 2.64, 95%CI 1.95-3.56) mortality. When accounting for incident multimorbidities after index date, RA was no longer associated with total (HR 1.08, 95%CI 0.96-1.20) or cardiovascular (HR 0.98, 95%CI 0.77-1.25) mortality, but excess respiratory mortality remained (HR 1.54, 95%CI 1.15-2.08). Seropositive RA remained associated with respiratory mortality before (HR 4.85, 95%CI 3.23-7.29) and after adjustment for all covariates (HR 2.13, 95%CI 1.54-2.94).
Conclusion: In this large prospective study using causal inference methods, excess total and cardiovascular RA mortality was explained by incident multimorbidities after diagnosis. For seropositive RA, excess respiratory mortality remained after accounting for measured lifestyle/clinical factors, emphasizing the importance of monitoring other factors (such as ILD, infections, or medications), that may mediate the RA respiratory mortality burden.
To cite this abstract in AMA style:
Sparks JA, Yoshida K, Lin TC, Camargo C, Raby B, Choi HK, Barbhaiya M, Tedeschi SK, Lu B, Costenbader K, Karlson E. Causal Inference Methods for the Effect of Rheumatoid Arthritis on Mortality Independent of Lifestyle and Clinical Factors before and after RA Diagnosis [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/causal-inference-methods-for-the-effect-of-rheumatoid-arthritis-on-mortality-independent-of-lifestyle-and-clinical-factors-before-and-after-ra-diagnosis/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/causal-inference-methods-for-the-effect-of-rheumatoid-arthritis-on-mortality-independent-of-lifestyle-and-clinical-factors-before-and-after-ra-diagnosis/