Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) carries a high risk for interstitial lung disease (ILD). Patients with SSc-ILD are prone to develop progressive lung fibrosis, but there are no validated algorithms for early detection of these patients. We assessed the frequency of progressive fibrosis in patients with SSc-ILD in the EUSTAR database and parameters associated with progression of fibrosis over a 12-month follow-up.
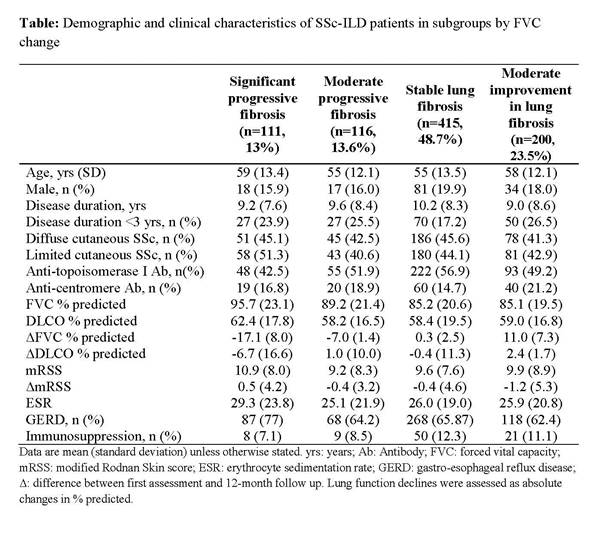
Methods: Patients registered in the EUSTAR database since 2010 who were ≥18 years old; fulfilled SSc classification criteria; had recordings for disease duration, baseline and 12+/- 3 months follow-up for lung function, and radiographic assessments for ILD (on HRCT or x-ray) were eligible for this longitudinal study. Significant progressive fibrosis was defined as FVC decline >10% or FVC decline 5-10% and DLCO decline ≥15% from baseline to a follow-up visit at 12+/- 3 months. Moderate progressive fibrosis was defined as FVC 5-10% decline without DLCO decline ≥15% over this time period. Significant improvement in fibrosis was defined as improvement of FVC > 10%, or improvement of FVC 5-10% and DLCO improvement ≥15% from baseline to a follow-up visit at 12+/- 3 months. Moderate improvement in fibrosis was defined as improvement in FVC ≥5-10% without DLCO improvement ≥15% over this time period. Stable lung fibrosis was defined as <5% change in either direction. Lung function declines were assessed as absolute changes in % predicted. Candidate predictors of significant progressive fibrosis were selected by expert opinion and logistic regression was applied.
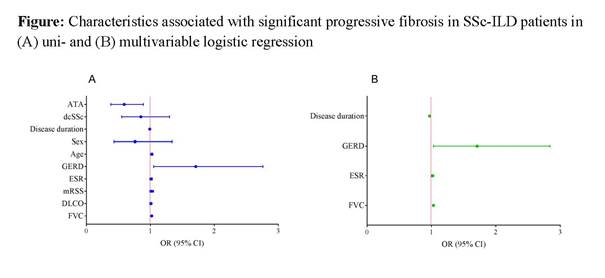
Results: A total of 826 SSc patients met the eligibility criteria including measurements for lung function after 12+/- 3 months follow-up. Of these, 106 (12.8%) showed significant progressive lung fibrosis, 113 (13.7%) moderate progressive lung fibrosis, 408 (49.4%) stable lung fibrosis, 189 (22.9%) moderate improvement in fibrosis and 10 (1.2%) significant improvement in fibrosis. Demographic and clinical characteristics by subgroup are shown in the Table. Baseline FVC, erythrocyte sedimentation rate (ESR), gastroesophageal reflux disease (GERD) and disease duration were significantly associated with the development of significant progressive fibrosis over 12+/- 3 months in uni- and multivariable modeling (AUC 0.67) (Figure). Age, sex, antibody profile and SSc subtype were not associated with significant progressive fibrosis in SSc-ILD.
Conclusion: This study provides novel insights regarding progressive fibrosis in patients with SSc-ILD in the large EUSTAR database.
To cite this abstract in AMA style:
Hoffmann-Vold AM, Allanore Y, Alves M, Graf N, Airò P, Ananyeva L, Czirják L, Guiducci S, Hachulla E, Li M, Mihai C, Sfikakis P, Valentini G, Kowal-Bielecka O, Distler O. Progressive Lung Fibrosis in Patients with Systemic Sclerosis-Associated Interstitial Lung Disease in the Eustar Database [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/progressive-lung-fibrosis-in-patients-with-systemic-sclerosis-associated-interstitial-lung-disease-in-the-eustar-database/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/progressive-lung-fibrosis-in-patients-with-systemic-sclerosis-associated-interstitial-lung-disease-in-the-eustar-database/