Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
Pulmonary arterial hypertension (PAH) is a severe complication of systemic lupus erythematosus (SLE), which is the most common underlying disease of CTD associated PAH. However its pathogenesis is still unknown. Both inflammatory mechanisms and endothelial dysfunction are involved. According to the guidelines, immunosuppressive therapy and pulmonary vasodilators were two common strategies in our clinical practice, but the responses to two therapies vary in different reports, indicating different underlying mechanisms in different patients. In order to identify homogeneous groups of SLE-PAH patients, we conducted this retrospective study.
Methods:
From 2011 to 2016 in Ren Ji Hospital, SLE-PAH patients were identified based on right heat catheterization (mPAP>=25 mmHg at rest, PAWP <15mmHg and PVR >3 WU) or echocardiography (peak tricuspid regurgitation velocity (TRV) >3.4m/s) excluding pulmonary hypertension due to left heart disease and pulmonary thrombosis. We distinguished two clusters according to multiple correspondence analysis and k-cluster analysis, which were defined as Vasculitic and Vasculopathic type. Kaplan-Meier survival curve of two clusters were made. Multivariate logistic regression was performed to identify predictors of clusters. Prediction model was established and ROC curve was made to find the optimal cut-off value.
Results:
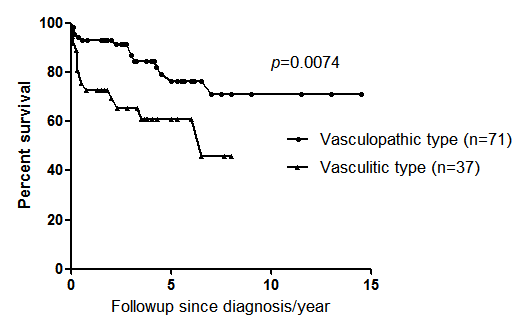
In a total of 108 SLE-PAH patients, two clusters with homogenous clinical features were identified. The Vasculitic Cluster were more likely to have pericarditis, LN, NPSLE, anemia, thrombocytopenia, as well as higher disease activity, and receiving higher doses of prednisone together with immunosuppressants, while the Vasculopathic type tended to have less systemic manifestations with lower disease activity, and were more likely given vasodilators in clinical practice. Overall, it seemed that the Vasculitic subtype was more severe with poorer outcome than the other subtype evidenced by the significantly higher mortality in survival curve (37.8% vs 18.3%, p=0.026) (Figure 1). Upon multivariate logistic regression, three predictors (SLEDAI > 9, hypertension and early onset of PAH < 2.99 years since SLE) were identified to distinguish Vasculitic SLE-PAH patients. Prediction model with these three factors were built, and ROC curve identified that score>=2 had a prediction rate of 89.5% with sensitivity of 91.9% and specificity of 94.4% (AUC 0.949, p<0.0001).
Conclusion:
In this retrospective cohort study, two clusters with different prognosis were identified. The Vasculitic type had more systemic manifestation and higher disease activity as well as poorer outcome than the Vasculopathic type. The prediction model combining three factors established in our study might help stratify the patients and guide the therapy in clinical practice.
Figure 1. Survival Curve of 108 SLE-PAH in two distinct clusters.
To cite this abstract in AMA style:
Sun F, Wu W, Guo L, Chen Z, Wang X, Li T, Ye S. Two Clinical Phenotypes of Chinese SLE-PAH Patients [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/two-clinical-phenotypes-of-chinese-sle-pah-patients/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/two-clinical-phenotypes-of-chinese-sle-pah-patients/