Session Information
Date: Sunday, October 21, 2018
Title: Muscle Biology, Myositis and Myopathies Poster I: Clinical Features and Disease Course
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Autoantibodies against melanoma differentiation-associated protein 5 (MDA-5) have been described in patients with dermatomyositis (DM) and progressive interstitial lung disease (ILD). Previous cohorts have shown a significant portion of these patients can develop rapidly progressive ILD. The goal of our study is to describe the phenotypic, physiologic, and radiologic features of this cohort and to identify important factors that may predict prognosis in terms of disease severity and outcomes.
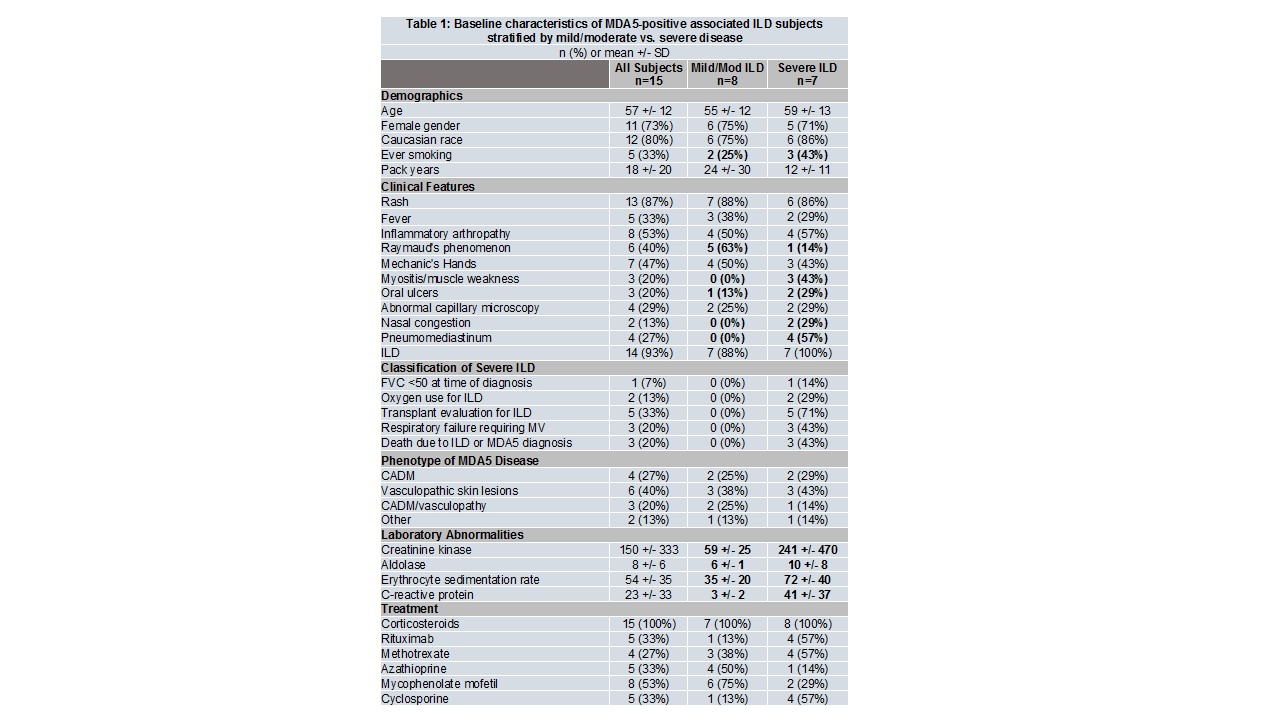
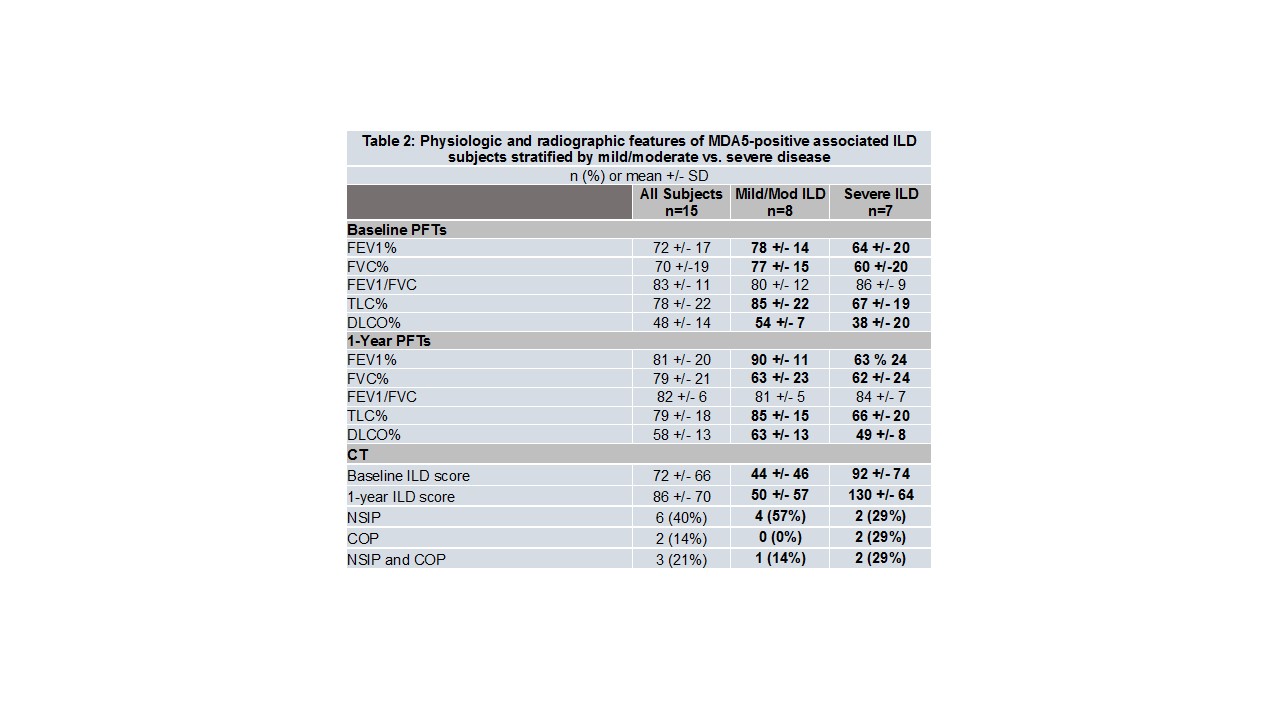
Methods: A retrospective single center observational longitudinal study characterized clinical characteristics, lung function, HRCT findings, and outcomes of MDA5-positive patients referred to a tertiary hospital. Patients who met the following criteria were defined as severe ILD: (1) baseline FVC <50% with ILD as known cause; (2) oxygen use due to ILD; (3) lung transplant evaluation due to ILD; (4) respiratory failure requiring mechanical ventilation for ILD; (5) death due to ILD or MDA5 diagnosis. CT scans were reviewed by 2 radiologists to determine ILD pattern and a semi-quantitative CT severity score.
Results: Fifteen MDA5-positive cases were identified between 2007 to 2018; 4 (27%) had clinically amyopathic DM (CADM), 6 (40%) had vasculopathic skin lesions, and 3 (20%) had both CADM/vasculopathy. Seven subjects (47%) developed severe ILD, of which 3 died from hypoxemic respiratory failure and 1 from failure to thrive. Those with severe disease had lower FVC%, TLC%, DLCO%, and CT ILD score at baseline and 1 year of following up, and were more likely to have a cryptogenic organizing pattern on CT. Smoking history, myositis, oral ulcers, nasal congestion, pneumomediastinum, and higher levels of inflammatory markers were more likely to be found in the severe group, whereas Raynaud’s phenomenon and non-specific interstitial pneumonia pattern on CT were more common in the mild/moderate group.
Conclusion: Our data supports that MDA5Ab-associated ILD seems to follow a bimodal pattern, which can be severe and/or progressive in a significant number of cases, but may be treatable and stabilized in certain patients. Although CADM and ulcerative and nodular lesions consistent with vasculopathy were found in equal frequency in the entire cohort and in the severe ILD subgroup, risk factors for severe disease appear to be smoking history, myositis, oral ulcers, nasal congestion, pneumomediastinum, and higher levels of inflammatory markers.
MDA-5 = melanoma differentiation–associated gene 5; CADM = clinically amyopathic dermatomyositis; ILD = interstitial lung disease
To cite this abstract in AMA style:
Doyle T, Borker P, Fletcher E, Murphy D, Madan R, Dellaripa PF. Clinical, Physiologic, and Radiologic Features Associated with Severe MDA5-Associated Interstitial Lung Disease [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/clinical-physiologic-and-radiologic-features-associated-with-severe-mda5-associated-interstitial-lung-disease/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/clinical-physiologic-and-radiologic-features-associated-with-severe-mda5-associated-interstitial-lung-disease/