Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
RA is associated with an increased risk of coronary artery disease (CAD). This association is believed to be due to systemic inflammation and its role in atherogenesis. The non-inflammatory FM has also been reported as an independent risk factor for CAD. In this study, we evaluated the outcomes of patients hospitalized for acute myocardial infarction (AMI) in those with and without RA or FM in a nationally representative sample.
Methods:
We used data from the National Inpatient Sample (NIS) for hospitalizations during the period 2005-2015 with adult AMI as the primary diagnosis and RA or FM as the secondary diagnosis using ICD-9 codes. The proportion who met ACR classification criteria cannot be determined with the NIS database. FM in the presence of immune-mediated or inflammatory rheumatic diseases was excluded. We used logistic regression to calculate the adjusted odds ratios for inpatient mortality from AMI with RA and with FM. We also investigated the unadjusted temporal trend of mortality rate in these groups and compared it to that of the general population.
Results:
We identified a total of 1,363,041 AMI hospitalizations from 2005-2015 of which 18,383 (1%) had a diagnosis of RA and 8133 (0.6%) had a diagnosis of FM. Compared to patients without RA, hospitalized RA patients were older (70.4 vs. 67.4 years; p<0.01) and predominantly female (62.8% vs. 39.1%; p<0.01). Compared to patients without FM, FM patients were younger (63.9 vs. 67.4 years; p <0.01) with an even higher proportion of females (81% vs. 39.1%; p<0.01).
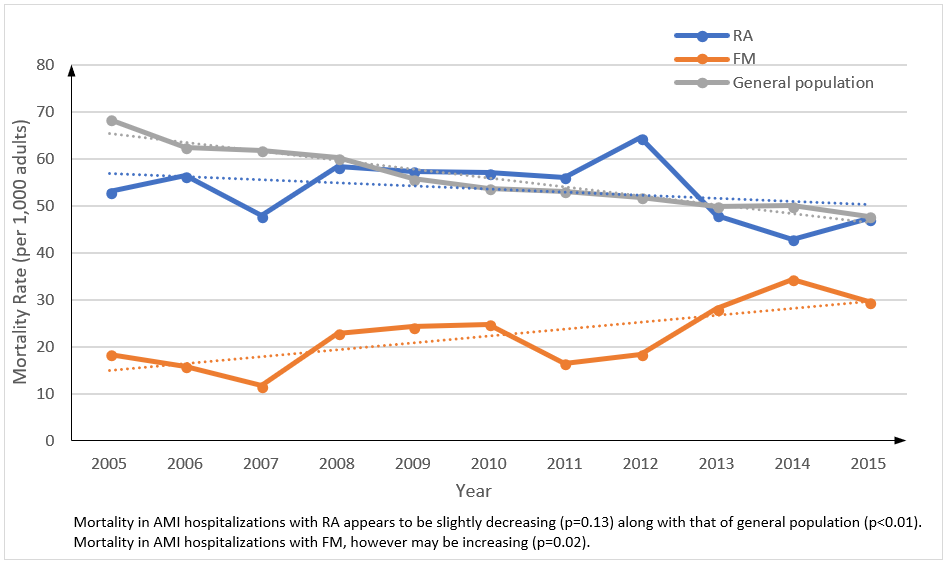
After adjusting for age, gender, race, comorbidities and cardiac procedures, RA hospitalizations with AMI had similar adjusted inpatient mortality (aOR=0.94; 95% CI= 0.87-1.01; p=0.14) compared to non-RA hospitalizations while the adjusted odds-ratio for inpatient mortality due to AMI in FM hospitalizations was 0.67 (95% CI= 0.57-0.80; p<0.01). The temporal trends of mortality rate (per 1,000 adults) in AMI hospitalizations in RA (p=0.13), FM (p=0.02) and the general population (p<0.01) are shown in the figure.
Conclusion:
Inpatient mortality in RA patients hospitalized for AMI was similar to that for non-RA patients even though the RA patients were older. The temporal trend of the unadjusted mortality rate in RA was similar to that of the general population and both were slightly decreasing. These findings may be related to strict cardiovascular risk factor modifications and in the case of RA, the availability of better DMARDs as well.
Compared to non-FM patients, patients with FM hospitalized for AMI had a lower inpatient mortality. The trend of AMI mortality rate in FM patients, however, was different from the other trends. Unlike that in RA or in general population, the AMI mortality rate in FM was increasing. This may be due to increased recognition of FM as a diagnostic entity or to the failure to recognize or treat CAD risk factors in the mostly female population.
To cite this abstract in AMA style:
Vafa A, Fugar S, Case JP. Outcomes of Hospitalizations and the Temporal Trends in Mortality from Acute Myocardial Infarction in Patients with RA and FM during 2005 to 2015 [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/outcomes-of-hospitalizations-and-the-temporal-trends-in-mortality-from-acute-myocardial-infarction-in-patients-with-ra-and-fm-during-2005-to-2015/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/outcomes-of-hospitalizations-and-the-temporal-trends-in-mortality-from-acute-myocardial-infarction-in-patients-with-ra-and-fm-during-2005-to-2015/