Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose:
Juvenile dermatomyositis (JDM) is an autoimmune disease that causes vasculopathy and inflammation of skin and muscles. Previous studies in adult dermatomyositis suggest increased risks of cardiovascular disease, but such assessments in JDM remain underexplored. This study evaluates cardiovascular risk factors and outcomes in children with versus without JDM.
Methods:
Data were analyzed from the 2002-2012 Nationwide Inpatient Sample, containing a representative 20% stratified sample of all hospitalizations in the United States. Primary (i.e. condition chiefly responsible for inpatient admission) vs secondary diagnoses of JDM (age <18 years) were identified using the previously validated ICD-9-CM code 710.3. Comorbidities were identified using ICD-9-CM codes in NIS for each patient discharge. Survey weighted logistic regression models were used to determine associations of JDM with comorbidities. Multivariate models included age, sex and race/ethnicity (model-1), as well as obesity, hypertension and diabetes (model-2) as binary covariates. A 2-sided p-value <0.05 was considered statistically significant.
Results:
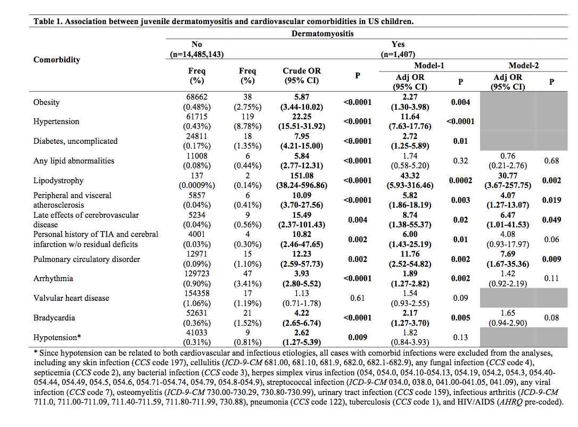
From 2002-2012, 909 primary and 498 secondary diagnoses of JDM were identified (from 14,535,620 pediatric hospital discharges). JDM inpatients were 34.6% male, 49.0% white, 18.5% black and 24.1% Hispanic. Twelve of 13 cardiovascular comorbidities were significantly associated with JDM (Table 1). Hypertension was the most common comorbidity in children with JDM (8.78% JDM patients vs 0.43% those without JDM, OR [95% CI]: 22.25 [15.51-31.92]). JDM was also associated with higher rates of obesity, uncomplicated diabetes, and lipid abnormalities. JDM inpatients had higher odds of cardio/cerebrovascular disorders, i.e. peripheral/visceral atherosclerosis, late effects of cerebrovascular disease, personal history transient ischemic attack/cerebral infarction, pulmonary circulatory disorder, arrhythmia, bradycardia, and hypotension. In multivariate regression models adjusting for age, gender and race/ethnicity, associations with JDM remained significant in 10 of 13 comorbidities.
Conclusion:
JDM is associated with higher odds of cardiovascular and cerebrovascular risk factors and disease. The possible interaction of chronic inflammation, vasculopathy, and treatment side effects with sociodemographic and cardiovascular risk factors requires further study.
To cite this abstract in AMA style:
Silverberg JI, Kwa L, Kwa MC, Laumann A, Ardalan K. Cardiovascular and Cerebrovascular Comorbidities of Juvenile Dermatomyositis in United States Children [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/cardiovascular-and-cerebrovascular-comorbidities-of-juvenile-dermatomyositis-in-united-states-children/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/cardiovascular-and-cerebrovascular-comorbidities-of-juvenile-dermatomyositis-in-united-states-children/