Session Information
Date: Wednesday, November 8, 2017
Title: Rheumatoid Arthritis – Clinical Aspects VI: Comorbidities of Rheumatoid Arthritis
Session Type: ACR Concurrent Abstract Session
Session Time: 9:00AM-10:30AM
Background/Purpose: Rheumatoid Arthritis (RA) is a multi-system disease which causes joint damage and is associated with increased cardiovascular (CV) morbidity and osteoporosis. Our purpose is to examine the relationship between bone mass and mortality in patients with RA.
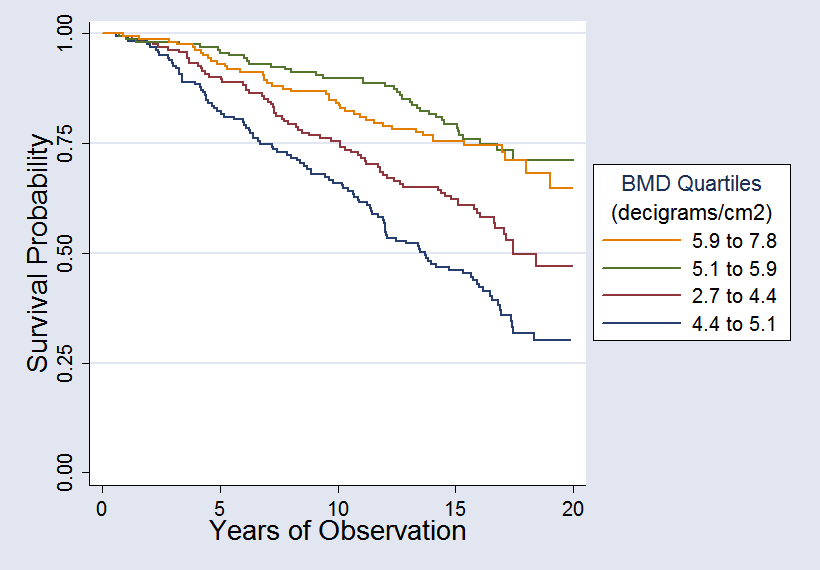
Methods: We recruited patients with RA from public and private rheumatology practices in San Antonio, Texas. In addition to demographic data, baseline measures were obtained including the extent and severity of joint involvement, the presence of CV risk factors (such as the presence of diabetes, tobacco use, hypercholesterolemia, and hypertension), and the bone mineral density (BMD), calculated from appendicular bone mass via Digital X-ray Radiogrammetry (DXR) of anteroposterior hand radiographs (Sectra AB, Linkoping, Sweden). During annual follow-up, all deaths were identified from relatives, physicians, obituaries, or national databases. We obtained certificates for all deaths. Patients were divided into groups according to BMD quartile. We used the Kaplan-Meier method to examine the association of BMD with mortality. We then adjusted for potential confounding variables using Cox proportional hazards regression analysis.
Results: Our study included 653 patients with RA. Their mean age ± standard deviation [SD] was 58.1±12.7 years and 72% were women. We had a total of 8,653 person-years [PY] of observation and noted 252 deaths over the course of the study for a mortality rate of 2.9 per 100 PY. Mortality was highest in the lowest BMD quartile at 5.2 per 100 PY (95% confidence interval [95% CI] 4.3-6.3). Higher BMD quartiles had less mortality, most notably in the two highest quartiles with a mortality rate of 1.9 per 100 PY (95% CI 1.4-2.6) and 1.6 per 100 PY (95% CI 1.2-2.2), respectively. The mortality hazard ratio (HR) was 0.74 per each decigram/cm2 increase in BMD (95% CI 0.62-0.90, P-value less than or equal to 0.01) after adjusting for age, sex, ethnicity, CV risk factors, and measures of RA inflammatory disease activity (counts of tender and swollen joints and erythrocyte sedimentation rate) and joint damage (Sharp score of radiographic erosions and joint space narrowing).
Conclusion: Low BMD in RA patients is independently associated with increased mortality rate. Together with other known risks factors and comorbidities, the presence of a low BMD suggests worse outcomes in patients with RA. BMD measurements via DXR may be of utility in the clinic as hand radiographs are routinely trended over time and readily obtained. Further research is needed to understand the mechanisms underlying the association between BMD and mortality in RA.
To cite this abstract in AMA style:
Hall ME, del Rincon I, Restrepo JF, Battafarano DF, Algulin J, Escalante A. Low Appendicular Bone Mass Predicts Mortality in Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/low-appendicular-bone-mass-predicts-mortality-in-patients-with-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-appendicular-bone-mass-predicts-mortality-in-patients-with-rheumatoid-arthritis/