Session Information
Date: Tuesday, November 7, 2017
Title: Rheumatoid Arthritis – Clinical Aspects Poster III: Comorbidities
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) increases atherosclerotic cardiovascular disease risk. Wave reflection occurs at arterial branching points, which are particularly prone to atherosclerosis. We hypothesised that wave reflection as assessed in separation analysis, represents atherosclerosis in RA.
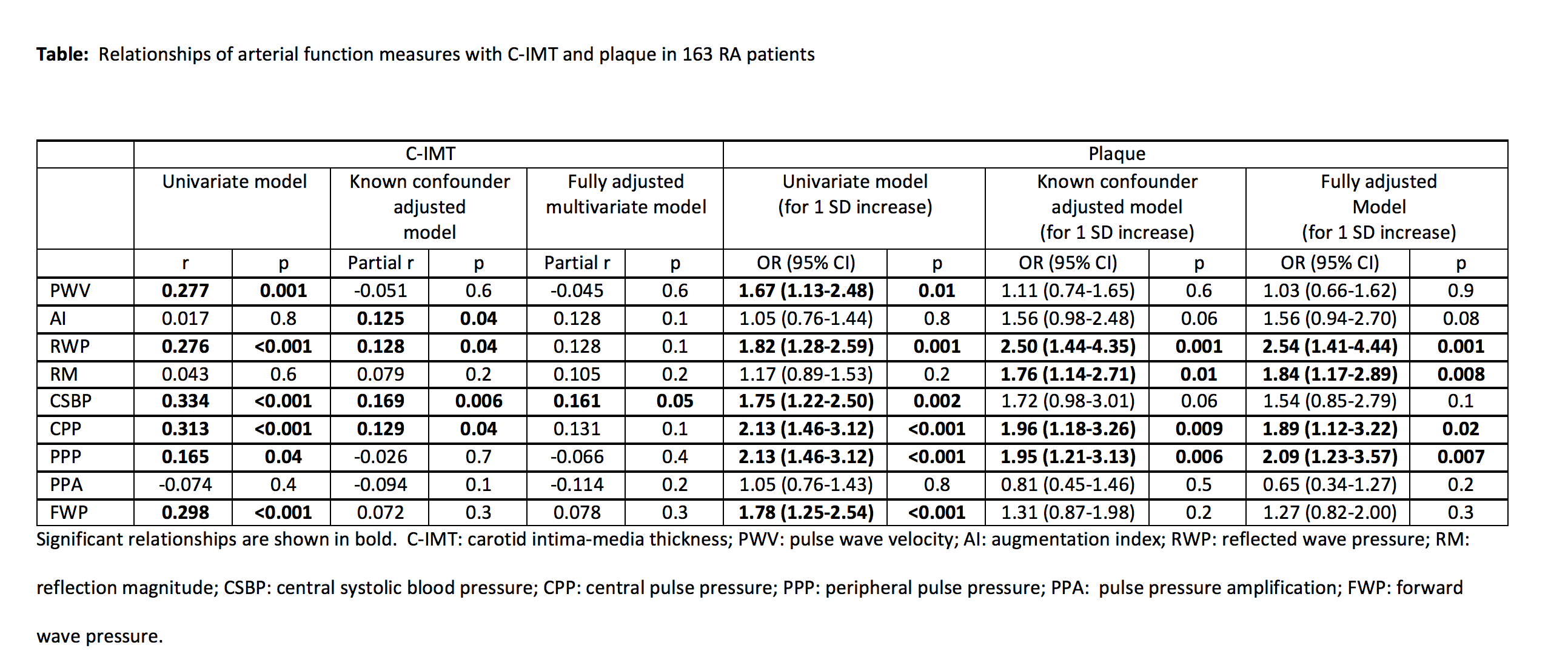
Methods: Confounder adjusted associations of SphygmoCor determined arterial stiffness (pulse wave velocity), wave reflection (augmentation index, reflected wave pressure and reflection magnitude) and pressure pulsatility (central systolic blood pressure, central pulse pressure, peripheral pulse pressure , pulse pressure amplification and forward wave pressure) with carotid plaque and intima-media thickness (c-IMT) on ultrasound were assessed in 163 RA patients (110 white, 31 Asian, 17 black and 5 of mixed ancestry) without cardiovascular disease. As age, sex, race, heart rate, body height, body weight and brachial mean blood pressure are established potential confounders in the present context, these characteristics were entered into each of the initial multivariable models (Table). Subsequently, other baseline characteristics that had bivariate associations with the arterial function variables were additionally entered as potential confounders in fully adjusted models on atherosclerosis (Table).
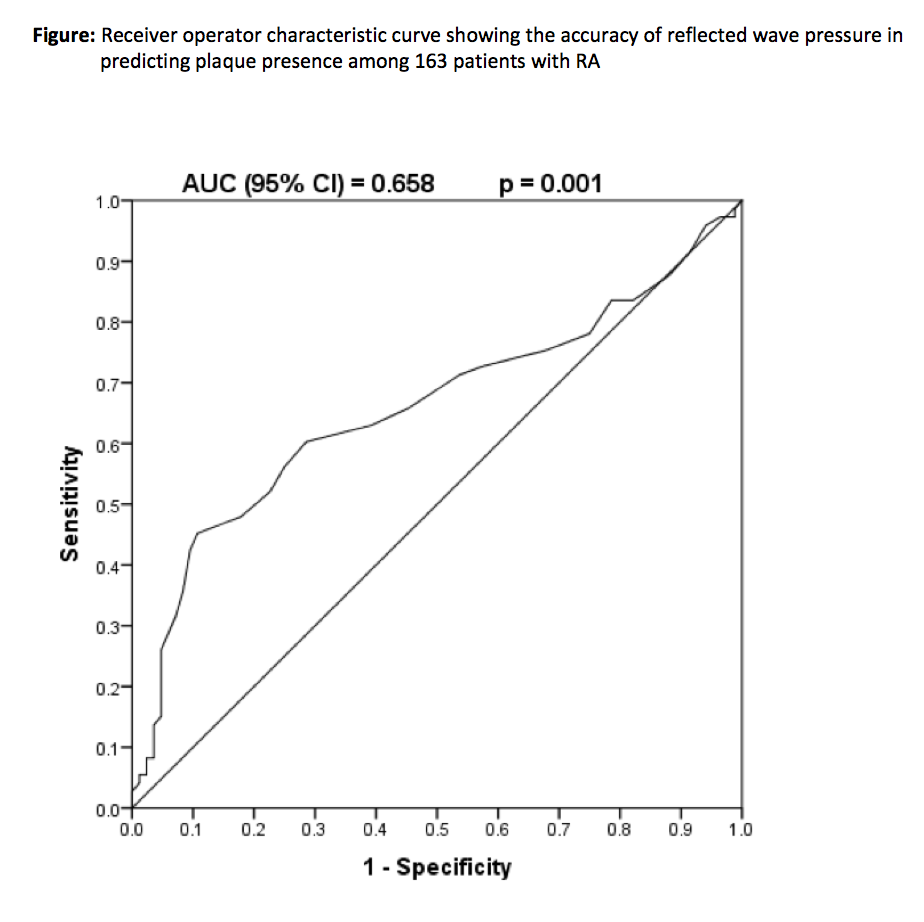
Results: One SD increase in reflected wave pressure (OR (95% CI) = 2.54 (1.41-4.44), p = 0.001), reflection magnitude (OR (95% CI) = 1.84 (1.17-2.89), p = 0.008), central pulse pressure (OR (95% CI) = 1.89 (1.12-3.22), p = 0.02) and peripheral pulse pressure (OR (95% CI) = 2.09 (1.23-3.57), p = 0.007) were independently associated with plaque (Table). The association of wave reflection with plaque was further independent of arterial stiffness and pressure pulsatility, and was present in both hypertensive and normotensive RA patients. In receiver operator characteristic curve analysis (Figure), the optimal cutoff value for reflected wave pressure in predicting plaque presence was 25 mm Hg with a sensitivity, specificity, positive predictive value and negative predictive value of 45.2%, 89.3%, 78.6% and 66.2%, respectively; a high reflected wave pressure increased the odds ratio for plaque 6.3 and 13.7 fold in univariate and adjusted analysis, respectively. Central systolic blood pressure (partial r = 0.161, p = 0.05) was independently related to c-IMT.
Conclusion: Increased wave reflection is associated with high risk atherosclerosis in RA. Consideration and therapeutic targeting of wave reflection may improve cardiovascular disease prevention in RA.
To cite this abstract in AMA style:
Gunter S, Robinson C, Woodiwiss A, Norton G, Hsu HC, Solomon A, Tsang L, Millen A, Dessein P. Arterial Wave Reflection and Subclinical Atherosclerosis in Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/arterial-wave-reflection-and-subclinical-atherosclerosis-in-rheumatoid-arthritis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/arterial-wave-reflection-and-subclinical-atherosclerosis-in-rheumatoid-arthritis/