Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Herpes zoster (HZ) is the painful reactivation of latent varicella zoster virus infection. The incidence of HZ may be increased in some autoimmune diseases including systemic lupus erythematosus (SLE). We examined the incidence and risk factors for HZ in a prospective cohort of patients with physician-diagnosed SLE compared to those diagnosed with non-inflammatory musculoskeletal conditions (MSK).
Methods: Study subjects were participants in the National Data Bank for Rheumatic Diseases (NDB) longitudinal study of rheumatic disease outcomes. Participants are followed prospectively with semi-annual detailed questionnaires collecting data on medication use, comorbid conditions, infections (including specific questions on HZ), hospitalizations, and standard patient reported outcomes. After excluding 808 participants with a history of prior HZ at enrollment, we followed 1,485 SLE patients and 2,775 MSK for incident HZ between 2001 and 2010. Reports of HZ were validated by confirmation of a physician diagnosis. Age adjusted incidence rates were calculated for each group. Cox proportional hazard regression models were used to identify predictors of HZ for the entire cohort as well as for specific predictors for SLE patients. Zostavax vaccination rates for individuals ≥ 60 years old were compared between groups.
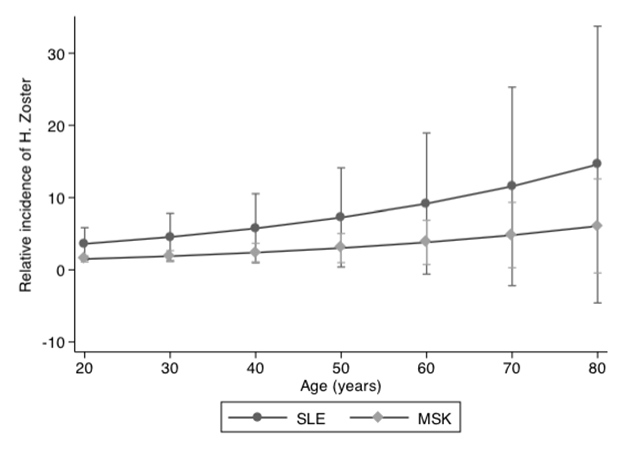
Results: SLE patients were younger than MSK (48.3 vs. 64.9 years), but had a similar disease duration of 13-14 years at enrollment. Health Assessment questionnaire at baseline was similar between groups (0.90 SLE vs. 0.87 MSK), although 25% of SLE patients were disabled from work compared to 9% of MSK. SLE patients had increased incidence of HZ at all ages, with an age-adjusted incidence of 12.0/1000 person-years compared to MSK (8.7/1000 person-years) and a hazard ratio of 1.7 (95% CI 1.08-2.71) for SLE (Figure). Increasing age (HR 1.01, 95%CI 1.00-1.02 per year) and increased HAQ (HR 1.26, 95% CI 1.10-1.44) were independent predictors of HZ. Among SLE patients, prednisone (HR 2.29, 95% CI 1.24-4.23) and mycophenolate mofetil (HR 5.00, 95% CI 1.40-17.6) conferred additional risk. SLE had the lowest HZ vaccination rates among age-eligible subjects; 7.1% SLE vs. 13% MSK, p<0.001.
Conclusion: The incidence of HZ is increased in SLE at all ages when compared to MSK, while vaccination rates remain low. Prednisone and mycophenolate mofetil are associated with increased risk.
Figure: Sex-adjusted relative incidence of incident herpes zoster by age for each diagnosis
Disclosure:
E. F. Chakarvarty,
None;
K. Michaud,
None;
R. S. Katz,
None;
F. Wolfe,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-incidence-of-herpes-zoster-among-patients-with-systemic-lupus-erythematosus/