Session Information
Date: Monday, November 6, 2017
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's – Clinical Aspects and Therapeutics Poster II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Interstitial lung disease (ILD) is a severe pulmonary complication associated with connective tissue diseases (CTDs), resulting in substantial morbidity and mortality. Despite advances in immunosuppressive drugs, there remains limited data on treatment for this challenging clinical entity. This study aims to evaluate the efficacy of rituximab (RTX) in patients with CTD-ILD and determine factors correlated with outcomes at 6 and 12 months post-RTX.
Methods:
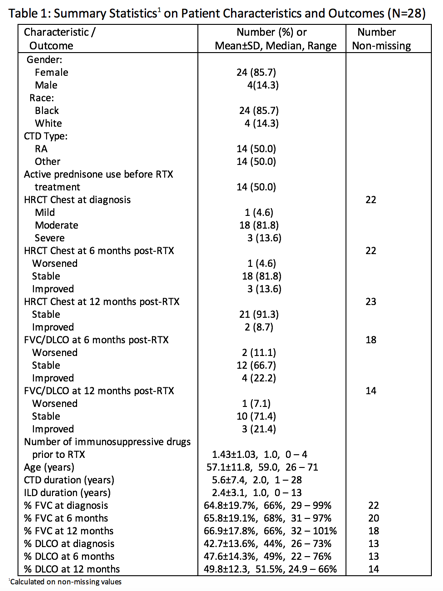
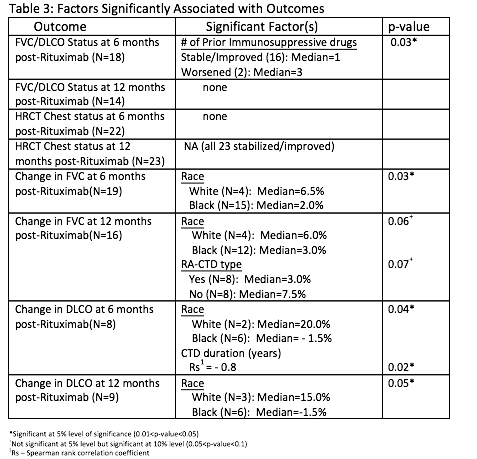
We analyzed data for 28 patients with CTD-ILD, all of whom met ACR classification criteria for a specific CTD. ILD was confirmed by high-resolution CT chest (HRCT) and pulmonary function tests with forced vital capacity (FVC) and diffusion capacity of lung for carbon monoxide (DLCO). We compared the HRCT chest findings, %FVC and %DLCO at time of diagnosis and at 6 and 12 months post-RTX treatment. We classified the HRCT chest findings at diagnosis into 3 groups, from mild to severe, and used the same semi-quantitative scoring system to evaluate for changes after treatment with RTX. We defined change in %FVC and %DLCO where improvement is an increase in FVC≥10% or DLCO ≥15%, worsening is a decrease in FVC≥10% or DLCO≥15% and stabilization is a change in FVC<10% or DLCO<15%. Multiple patient characteristics (Table 1) were tested for their correlations with each outcome using separate univariate analysis with the chi-square/Fisher test or Wilcoxon rank sum test.
Results:
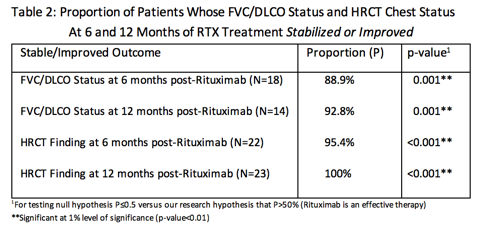
Majority of the patients were female and African American with median age of 59. The median duration for CTD and ILD was 2 years and 1 year, respectively (Table 1). The proportions of patients whose FVC, DLCO and HRCT Chest status remained stable or improved post-RTX at 6 and 12 months were all significantly higher than 50% (Table 2). Furthermore, the proportions of patients who remained stable or improved were higher at 12 months than at 6 months. The median %change in FVC at 6 months was +3% and at 12 months was +3.5%. The median %change in DLCO at 6 months was +1.5% and at 12 months was +7%. Race, prior immunosuppressive drugs and CTD duration were all significantly associated with the observed outcomes (Table 3).
Conclusion:
Based on this single center retrospective study, RTX appears to be an acceptable and effective therapy for CTD-ILD. RTX may help to fill an unmet therapeutic need for CTD-ILD and larger randomized clinical trials are needed.
To cite this abstract in AMA style:
Patel S, Hayat S, Caldito G, Erickstad K. Efficacy of Rituximab for Connective Tissue Disease-Associated Interstitial Lung Disease: A Single Center Study of 28 Patients [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/efficacy-of-rituximab-for-connective-tissue-disease-associated-interstitial-lung-disease-a-single-center-study-of-28-patients/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/efficacy-of-rituximab-for-connective-tissue-disease-associated-interstitial-lung-disease-a-single-center-study-of-28-patients/