Session Information
Date: Monday, November 6, 2017
Title: Systemic Lupus Erythematosus – Clinical Aspects and Treatment Poster II: Damage and Comorbidities
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic lupus erythematosus (SLE) is heterogeneous in its clinical prognosis and lupus nephritis (LN) is a major cause of morbidity and mortality among children and adults with SLE. LN patients typically receive higher doses of corticosteroids (CS) than do non-renal SLE patients. The excess burden of disease and treatment on hospitalization and in-hospital death associated with SLE and LN remains incompletely understood. This study characterized rates of hospitalizations, CS-related reasons for hospitalization, and in-hospital mortality of SLE and LN pts compared to: 1) each other; 2) matched controls.
Methods: Retrospective cohort study using the Truven Healthcare MarketScan® Commercial Claims and Encounters and Medicare Supplemental and Coordination of Benefits database from 1999 to 2014. LN and SLE cohorts were based on validated algorithms using claims data.1,2 Controls with claims for non-autoimmune conditions were matched on age and gender at index date. All pts had ≥ 365 days of enrollment ± index date. End of study was the first of end of enrollment or database, or date of death. Potentially CS-related reasons for hospitalization were evaluated on a claims-based modification of adverse events (AEs) on a CS toxicity index.3
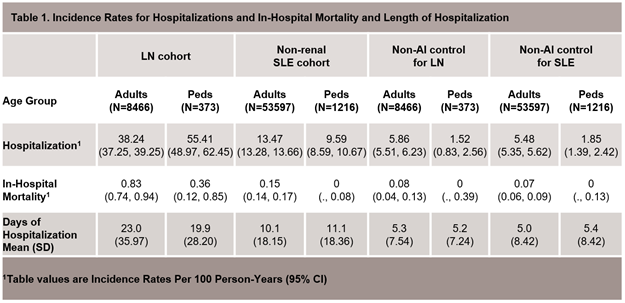
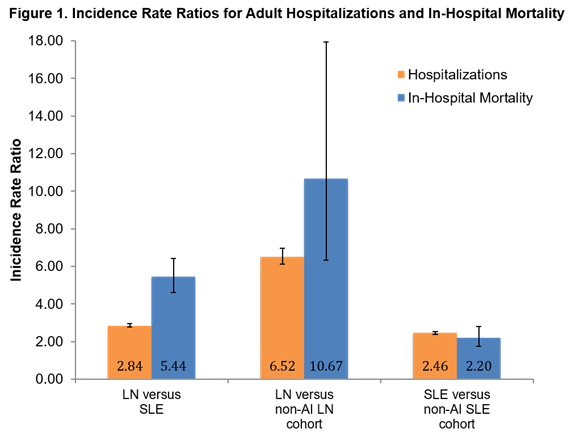
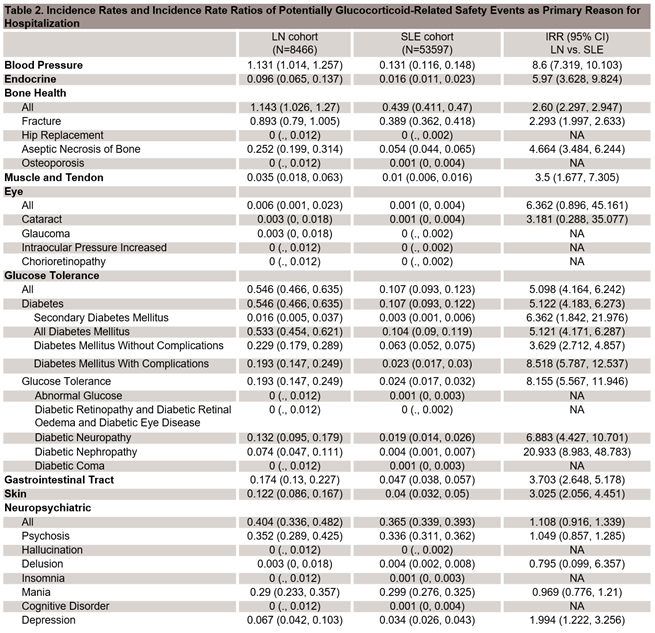
Results: 54,813 SLE pts w/o renal involvement and 8,839 LN pts were identified. LN adults had the longest hospitalizations (Table 1); Incidence rate ratios (IRRs) confirm statistically significantly higher rates of hospitalization and in-hospital mortality for LN compared to SLE and for both disease groups compared to controls (Figure 1). LN was associated with increased incidence of several potentially CS-related AEs (e.g. diabetes, aseptic necrosis of bone, depression) as the primary reason for hospitalization compared with the non-renal SLE group (Table 2).
Conclusion: The medical need for safe and effective treatments of LN and SLE remains unmet. The retrospective, claims-based results do not permit pt-level assessment of the relative contributions of disease severity, treatment, and other potential confounders of these findings. Ongoing analyses are examining the role of steroid exposure on CS-related hospitalizations.
1. Arkema EV et al. BMJ Open, 2016;6:e007769.
2. Chibnik LB et al. Lupus, 2010;19:741-3.
3. Miloslavsky EM et al. Ann Rheum Dis, 2016;76:543-6.
To cite this abstract in AMA style:
Belendiuk K, Trinh H, Cascino M, Dragone L, Keebler D, Garg J, Brunetta P. Lupus Nephritis Is Associated with Increased Rates of Hospitalization for Adverse Events on a Glucocorticoid Toxicity Index and in-Hospital Mortality Compared with Non-Renal Lupus and Matched Controls: An Analysis of Insurance Claims Data [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/lupus-nephritis-is-associated-with-increased-rates-of-hospitalization-for-adverse-events-on-a-glucocorticoid-toxicity-index-and-in-hospital-mortality-compared-with-non-renal-lupus-and-matched-controls/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-nephritis-is-associated-with-increased-rates-of-hospitalization-for-adverse-events-on-a-glucocorticoid-toxicity-index-and-in-hospital-mortality-compared-with-non-renal-lupus-and-matched-controls/