Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Women with primary Sjögren’s syndrome (pSS) often experience vaginal dryness. The cause of this symptom is unknown. This study compared the vaginal and cervical health of women with pSS and controls, using clinical and histopathological parameters.
Methods: Consecutive premenopausal women with pSS according to the AECG and ACR-EULAR criteria, with symptoms of vaginal dryness, and age-matched controls planned for a risk-reducing salpingo-oophorectomy underwent a vaginal examination. Excluded were women with an inflammatory or infectious gynaecological disease, intra-uterine contraceptive device, or use of hormone therapy or DMARDs. Participants were screened for chlamydia, gonorrhea, and vaginal bacterial and fungal infections. The vaginal health index was recorded, which consists of 5 domains (elasticity, fluid secretion, pH, epithelial mucosa, moisture). Each domain was scored on a scale of 1-5, resulting in a score of 5-25. Low scores correspond to low vaginal health. In pSS patients, vaginal and endocervical biopsies were taken under local anesthesia. In controls, the investigation was performed under general anesthesia, prior to surgery. Formalin fixed and paraffin embedded tissue sections were stained for HE and CD45 (leucocytes) and examined by a dedicated gynaecopathologist. The percentage of area stained for CD45 was calculated with Aperio ImageScope v12.0. Groups were compared using Mann-Whitney U test.
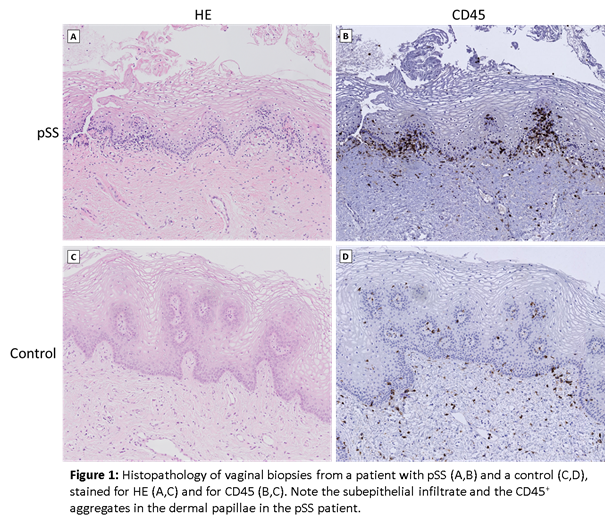
Results: A total of 9 pSS patients and 5 controls were included so far. One pSS patient was excluded from the analysis due to presence of Chlamydia trachomatis. Median age was 35 years (IQR 30-46) in pSS patients and 37 years (IQR 36-42) in controls (p=0.62). Median vaginal health index was lower in pSS patients (18.5, range 14-23) compared to controls (23.0, range 20-23, p=0.019). In the HE staining of the vaginal tissue, a mild (n=6) or moderate (n=2) infiltrate was seen in all pSS patients. In controls, no infiltrate (n=3) or a mild infiltrate (n=2) was seen in the vaginal tissue. Infiltrates were mainly located in the subepithelial layer, with aggregates in dermal papillae (figure 1). The median percentage of area stained for CD45 in the vagina was higher in pSS patients (2.0%, range 1.0-5.0%) compared to controls (1.4%, range 0.4-1.4%, p=0.03). Endocervical tissue was obtained in 5 pSS patients and in 3 controls. In the HE staining of the endocervical tissue, moderate or severe infiltrates were seen in 3 pSS patients, and a moderate infiltrate in 1 control. The median percentage of area stained for CD45 in the endocervix did not differ between groups (patients 4.4%, range 1.1-28.3%; controls 3.2%, range 2.0-13.0%, p=1.00).
Conclusion: In this preliminary analysis, pSS patients show a lower vaginal health index and a higher percentage of subepithelial infiltrate in the vagina compared to controls, while endocervical histopathology did not differ. Detailed phenotypic evaluation of the infiltrate will follow.
To cite this abstract in AMA style:
van Nimwegen JF, van der Tuuk K, Klinkert ER, Haacke EA, Kroese FGM, Hollema H, Mourits MJ, Bootsma H. Subepithelial Infiltrate of the Vagina in Primary Sjogren’s Syndrome: The Cause of Vaginal Dryness? [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/subepithelial-infiltrate-of-the-vagina-in-primary-sjogrens-syndrome-the-cause-of-vaginal-dryness/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/subepithelial-infiltrate-of-the-vagina-in-primary-sjogrens-syndrome-the-cause-of-vaginal-dryness/