Session Information
Title: Rheumatoid Arthritis - Clinical Aspects I: Risk Factors and Prediction of Rheumatoid Arthritis
Session Type: Abstract Submissions (ACR)
Background/Purpose:
The first hurdle general practitioners (GPs) face to identify Rheumatoid Arthritis(RA) is to recognize presence of arthritis. Due to the low incidence of arthritis in primary care it is challenging to differentiate between patients with inflammatory musculoskeletal disease and those without . We set out to create a referral model to aid early referral in primary care based on data from the REACH.
Methods:
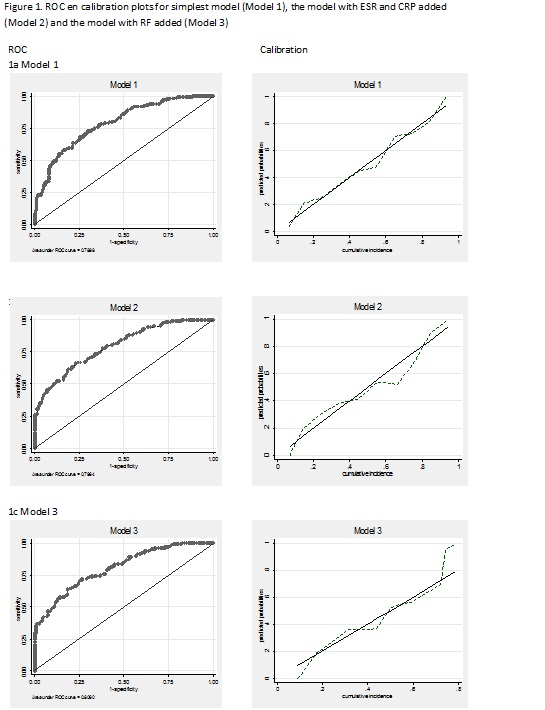
The REACH cohort includes patients with either arthritis or 2 painful joints with 2 additional inflammatory characteristics. Four hundred and one patients referred to REACH by their GPs were used in this analysis. A prediction model was build by selection of variables from the history, physical examination and laboratory values that were likely available to GPs. The presence of at least one joint with synovitis was used as outcome excluding patients with gout. Variable selection was performed by classifying variables in 8 categories: symptoms, duration of complaints, life style, family history, comorbidity, medication use and systemic complaints (fever, skin disorder) followed by logistic regression with backward selection in each category. A referral model was build with the variables with p<0.1 evaluated in a logistic regression model that was bootstrapped 200 times to elicit the for optimism corrected c-statistic. Performance was also evaluated using ROC-curves and calibration plots. The addition of blood markers to the simple model was also evaluated.
Results:
Table 1 shows baseline characteristics for the 401 patients. Arthritis was present at baseline in 182 patients. The referral model based on the REACH data resulted in a model containing the following variables: age, female sex, problems with fitting shoes, self-reported limitation of joint movement, lower number of self-reported painful joints, higher number of self-reported swollen joints, self-reported redness or hot/warm joints, the presence of squeeze pain in hand or feet and delay in presenting to the GP. The AUC was 0.79 (corrected for optimism: 0.72), adding ESR resulted in an AUC of 0.80 and adding RF resulted in 0.81. The simplest model calibrated slightly better (fig 1).
Conclusion:
We were able to create a referral model based on history taking and physical examination suitable for referral of patients with arthritis at risk for RA and perhaps other inflammatory diseases in primary care. Adding laboratory values did not improve performance and thus may be omitted based on the resources of the primary care facility.
Table 1. baseline characteristics
|
|
case, n=182 |
non case, n=219 |
|
|
|
age (mean, SD) |
51 (15) |
47 (12) |
p<0.05 |
|
|
gender (%) |
69% |
66% |
p<0.05 |
|
|
duration of complaints (median, range) |
68 (4-370) |
122 (1-416) |
p<0.05 |
|
|
delay patient (median, range) |
21 (0-328) |
43 (0-361) |
p<0.05 |
|
|
tender joint count (median, range) |
7 (0-34) |
6 (0-38) |
ns |
|
|
rheumatoid factor posistive (%) |
25% |
11% |
p<0.05 |
|
|
anti-CCP positive (%) |
17% |
6% |
p<0.05 |
* |
|
ESR (median, range) |
18(2-100) |
8(0-66) |
p<0.05 |
@ |
|
C-reactive proteine (median, range) |
6 (1-180) |
3 (1-55) |
p<0.05 |
# |
|
Diagnosis RA |
0% |
29% |
p<0.05 |
$ |
* n=30 missing, @ n=63 missing, # n=92 missing, $ n=47 missing
Disclosure:
C. Alves,
None;
J. J. Luime,
None;
D. P. Shackleton,
None;
P. J. Barendregt,
None;
A. H. Gerards,
None;
J. M. W. Hazes,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-easy-to-use-referral-model-for-arthritis-from-the-rotterdam-early-arthitis-cohort/