Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose:
While extensive studies have been performed to characterize ANCA, little is known about the auto-reactive B cells that produce these autoantibodies. Indirect evidence previously suggested the presence of circulating PR3-specific B cells in patients with PR3-ANCA-associated vasculitis (AAV). Our objectives here were to develop a method to detect circulating PR3-specific B cells in patients with PR3-AAV, to study their proportion among the different B-cell subsets and to assess their relationship with disease activity.
Methods:
A recombinant PR3 (rPR3) was tagged using FITC or biotin, and we studied its ability to bind specifically to two hybridoma cell lines, MCPR3-2 (producing an anti-human PR3 monoclonal antibody) and MCPR3-13 (producing an anti-mouse PR3 monoclonal antibody, with no cross-reactivity with human PR3). We measured the proportion of PR3-FITC positive B cells among PBMCs in 13 patients with PR3-AAV and 14 healthy controls (HCs) by flow cytometry. We then developed a multi-color flow cytometry including CD19, IgD, CD27, CD38, CD24 and biotinylated rPR3 to measure the proportion of PR3-specific B cells among different B-cell subsets in an independent group of 13 patients with PR3-AAV and 11 HCs.
Results:
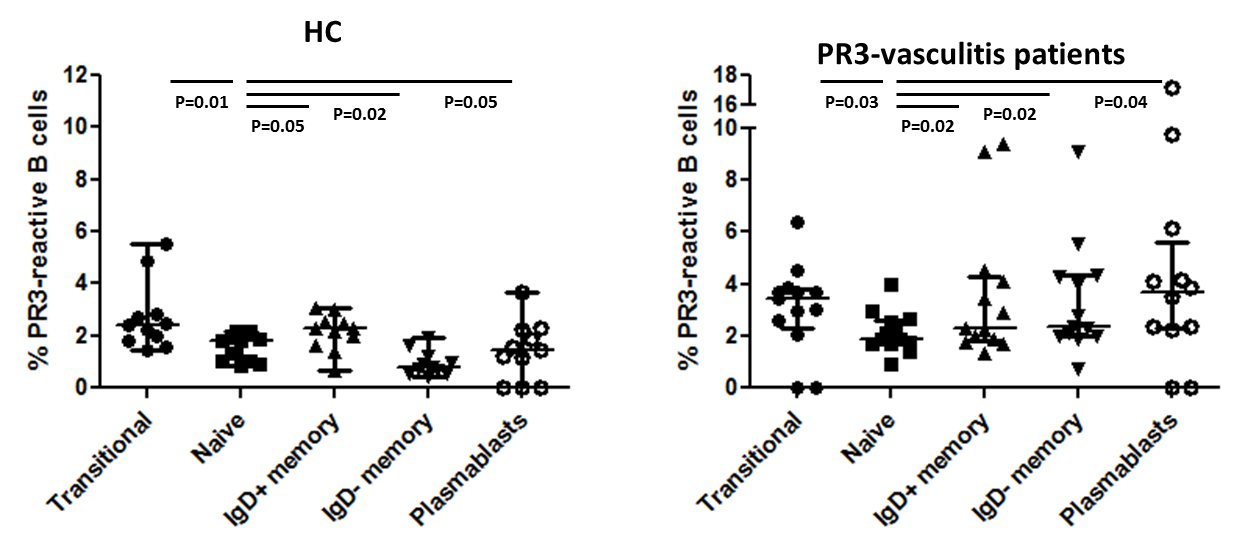
rPR3 efficiently bound MCPR3-2 hybridoma cells but not MCPR3-13. Specificity of the staining was confirmed by competition experiments: pre-incubation of MCPR3-2 cells with untagged human rPR3 totally abrogated rPR3-FITC staining, whereas pre-incubation with mouse rPR3 had no effect. Dose-ranging experiments defined the optimal concentration of rPR3 to stain cells expressing anti-PR3 immunoglobulin. The mean (SEM) proportion of rPR3-FITC-stained B cells was higher in patients with PR3-AAV compared to HCs: 2.10% (2.33) vs 0.45% (0.19) respectively, p<0.001. Patients with active disease had numerically higher proportions of PR3-specific B cells than patients in remission: 3.66% (3.28) vs 1.10% (0.52), p=0.09. In HCs, the proportion of PR3-specific B cells was highest among the transitional B-cell subset, and decreased along with the maturation of B cells (figure). Conversely, in patients, the proportion of PR3-specific B cells progressively increased with the maturation of B cells (median 1.9% of naïve B cells, 2.30% of IgD+ memory B cells, 2.37% of IgD- memory B cells, and 3.68% of plasmablasts, p<0.05 for all comparisons with the naïve subset).
Conclusion:
This study describes an original method to detect and study circulating auto-reactive B cells in patients with PR3-AAV, and suggests that PR3-specific B cells are associated with disease activity and may represent a promising biomarker to predict relapse risk in patients in clinical remission. The progressive enrichment in PR3-specific B cells during the B-cell maturation steps in patients suggest that auto-reactive B cells are actively selected and escape peripheral tolerance checkpoints.
To cite this abstract in AMA style:
Cornec D, Berti A, Hummel A, Peikert T, Pers JO, Specks U. Auto-Reactive B Cells Escape Peripheral Tolerance Checkpoints in Patients with PR3-ANCA Associated Vasculitis [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/auto-reactive-b-cells-escape-peripheral-tolerance-checkpoints-in-patients-with-pr3-anca-associated-vasculitis/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/auto-reactive-b-cells-escape-peripheral-tolerance-checkpoints-in-patients-with-pr3-anca-associated-vasculitis/