Session Information
Date: Wednesday, November 16, 2016
Title: Epidemiology and Public Health III: Psoriatic Arthritis and More
Session Type: ACR Concurrent Abstract Session
Session Time: 11:00AM-12:30PM
Background/Purpose:
Smoking is a strong risk factor for psoriasis and psoriatic arthritis, but several studies have found that smoking is inversely associated with the risk of psoriatic arthritis (PsA) among psoriasis (PsO) patients. These paradoxical findings may occur due to index event bias (a selection bias also called collider bias) that arises from selecting a group of patients (e.g., PsO) on the causal pathway (e.g., between smoking and PsA), such that the total effect of smoking on risk of PsA among PsO patients cannot be appropriately assessed using conventional methods. Moreover, the obtained direct effect (i.e., effect of smoking on the risk of PsA not through PsO) may also be biased. We sought to confirm the paradox in a substantially larger sample and conduct sensitivity analyses to quantify the potential bias on the direct effect estimate.Methods: We used 1995-2015 data from The Health Improvement Network (THIN), an electronic medical record database representative of the UK general population. We analyzed data from adults free of PsA after at least 1 year of enrollment into THIN, and with data on factors of interest. Follow-up began with the first record of smoking status (exposure) after the enrollment period and ended at the time of PsA diagnosis, death, loss to follow-up, or the end of the study, whichever came first. Using Cox regression, we assessed the effect of smoking on incident PsA in the general THIN population and then in patients with PsO. We conducted a “bias sensitivity analysis” for a range of possible relative risks for the association between smoking and potential unmeasured confounders “U” (e.g., genetic factors) and that between U and PsA. Analyses were adjusted for baseline confounders.
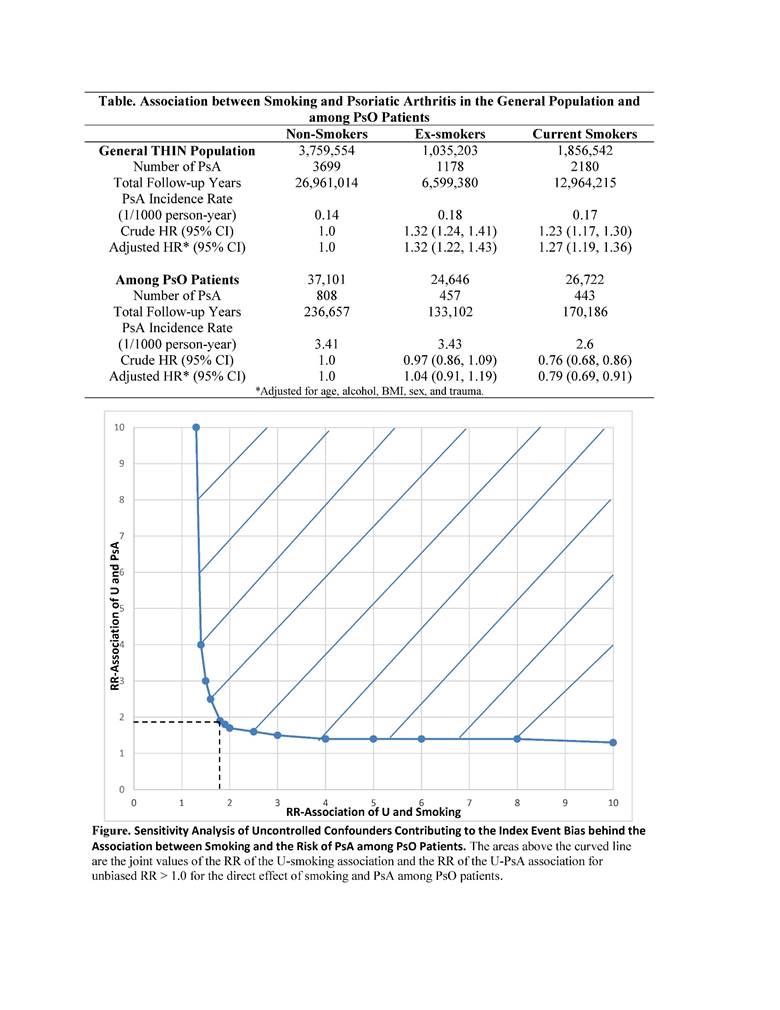
Results: There were over 6.6 million subjects without PsA at baseline (mean age 42 years; 53% female; 28% current smokers, and 16% ex-smokers). Of those, 88,469 developed incident PsO, among whom 1,708 developed incident PsA. The adjusted hazard ratio (HR) of smoking for the risk of PsA among PsO patients was 0.79 (95%CI: 0.69, 0.91), but the corresponding HR for PsA in the general THIN population was 1.27 (95%CI: 1.19, 1.36) (Table). Results from the bias sensitivity analysis indicated that if the association between U and smoking and that between U and PsA were as low as a relative risk (RR) of 1.8 and 1.9, respectively, then it could nullify a biased protective effect (RR=0.8) (Figure).
Conclusion: This large cohort study confirms that conditioning on PsO can reverse the true association between smoking and PsA. Such index event bias can produce a misleading estimate of the impact of modifiable risk factors. We suggest that investigators perform sensitivity analyses to assess how sensitive the observed effect estimate is to unmeasured confounding and its associated index event bias.
To cite this abstract in AMA style:
Nguyen USDT, Zhang Y, Felson DT, Lavalley MP, Choi HK. Sensitivity Analysis for the Smoking Paradox in the Development of Psoriatic Arthritis Among Psoriasis Patients [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/sensitivity-analysis-for-the-smoking-paradox-in-the-development-of-psoriatic-arthritis-among-psoriasis-patients/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sensitivity-analysis-for-the-smoking-paradox-in-the-development-of-psoriatic-arthritis-among-psoriasis-patients/