Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: PROMIS-29 is a generic health-related quality of life (HRQoL) instrument that was developed as part of the NIH Patient Reported Outcomes (PROs) Roadmap. Our objective was to assess the construct validity of PROMIS-29 in participants with SSc-ILD.
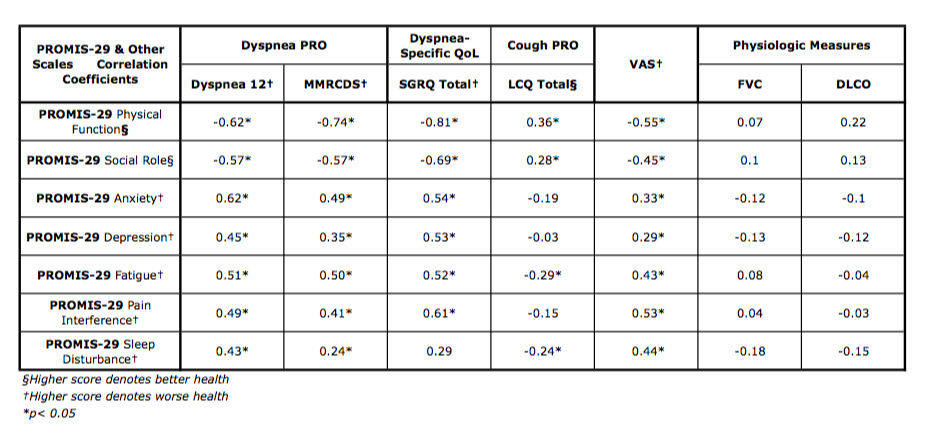
Methods: Ninety-four participants with SSc were recruited from a large Scleroderma Program. Participants included in the study satisfied 2013 ACR/EULAR criteria for SSc and had ILD on HRCT. Participants with FEV1/FVC less than 0.7 were excluded from study. At baseline, participants were administered PROs, consisting of PROMIS-29, Patient global assessment for disease severity on a visual scale (VAS), Dyspnea 12, Modified Medical Research Council Dyspnea Scale (MMRC; dyspnea measure), Leicester Cough Questionnaire (LCQ; cough measure), and the Saint George Respiratory Questionnaire (SGRQ; respiratory disease impact measure). Along with PROs, pulmonary function test (PFT), HRCT, medical history, physical exam, and medications data were obtained. PFT indices (forced vital capacity and DLCO) were compared across PROÕs. Pearson correlation coefficients were calculated and interpreted as proposed by Cohen: 0.0 – 0.10 indicates negligible correlation, 0.10 – 0.23 indicates a small correlation coefficient, 0.24 – 0.36 indicates a moderate correlation, 0.37 is indicative of a large correlation coefficient.
Results: The mean age of participants was 51.6 years, with a mean disease duration of 2.8 years after first non-ReynaudÕs symptom. Of the 94 participants, 60.6% were classified as diffuse SSc, 24.5% limited SSc, 13.8% sine, and 1.1% overlap. Mean FVC was 74.9%, DLCO was 53.5% and 88% had NSIP fibrotic pattern on HRCT. PROMIS-29 scores were 0.2 to 0.9 SD below the US population. Correlation coefficients were highest with PROMIS physical function scale (0.36 to -0.81 for all comparisons; p< 0.05). Correlations were higher for dyspnea scales compared to LCQ. The correlation coefficients with physiologic measures (FVC and DLCO) showed negligible-to-small coefficient vs. PROMIS measures.
Conclusion: PROMIS-29 has construct validity for assessment of HRQoL in SSc-ILD. It has moderate-to-large correlations with measures of dyspnea, dyspnea-specific QoL, and cough, and complements physiologic measures. We are currently assessing sensitivity to change in the longitudinal cohort.
To cite this abstract in AMA style:
Fisher C, Namas R, Young A, Wilhalme H, Khanna D. Performance of the Patient-Reported Outcomes Measurement Information System (PROMIS) 29 in Systemic Sclerosis -Associated Interstitial Lung Disease (SSc-ILD) [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/performance-of-the-patient-reported-outcomes-measurement-information-system-promis-29-in-systemic-sclerosis-associated-interstitial-lung-disease-ssc-ild/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-the-patient-reported-outcomes-measurement-information-system-promis-29-in-systemic-sclerosis-associated-interstitial-lung-disease-ssc-ild/