Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Flares are a common experience in RA, often associated with worse clinical outcomes such as cardiovascular disease, lower functional status, and radiographic progression. Many flares develop between rheumatology visits, thus little is known about management strategies. This study aims to examine which strategies contribute to a successful post flare outcome.
Methods: Data from 317 patients enrolled in a prospective RA registry were collected, including clinical and patient reported outcomes. Patients completed a flare survey asking about frequency, outcomes, and management; including a Likert scale assessing if post flare symptoms were better, unchanged, or worse (Figure 1). Ordinal logistic regression analysis adjusting for age, sex, number of flares in past 6 months, severity of most recent flare (0-10), home management, clinical treatment, and medication change was performed with symptoms post flare as the outcome.
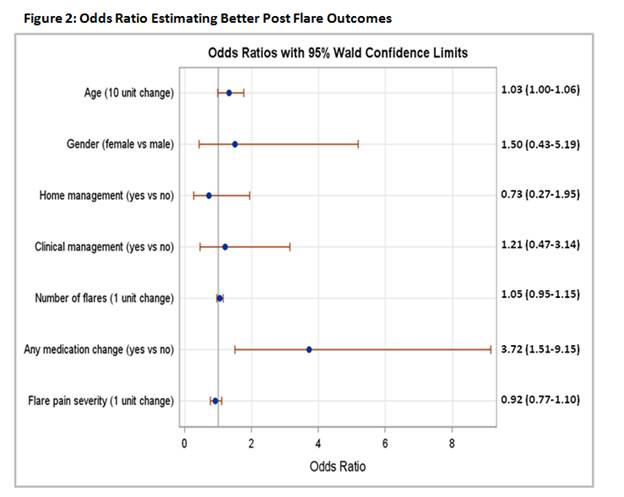
Results: 114 patients had a flare that had ended (87.7% female, mean age 59 (±14.2) years, median disease duration 14 (IQR 9, 24) years). Median flare severity was 7 (5, 8). Compared with RA symptoms before the flare, 16 (14%) patients reported worsened RA symptoms post flare, 71(63%) were unchanged, and 26 (23%) were improved. To manage flares, 90 (79%) patients used home management (e.g. ice/heat (53%) and rest (61%)), and 58 (51%) reported making a medication change (50% NSAIDs, 32% corticosteroids, 26% DMARDs). Only 30 (26%) patients sought clinical advice (e.g. rheumatologist (87%) and PCP (7%)). Of note, 59% of patients who made a medication change did so without seeking clinical advice. The logistic model (Figure 2) revealed that patients who made a medication change, of any kind, to treat their flare were more likely to have improved RA symptoms post flare than patients who made no medication change (OR=3.715, p=0.004). No other covariates were significant, including flare frequency and severity. In a sub analysis, individual medication category did not influence post flare outcome.
Conclusion: Independent of home based or clinically guided care, making a medication change is strongly associated with improved post flare outcomes. This improvement was not attributable to any one category of medication and the decision to make a medication change was frequently made without seeking clinical advice. This has implications for understanding how best to intervene when patients flare. Future directions could examine if specific medication changes in combination with home or clinical management strategies facilitate better post flare outcomes. Figure 1: RA Symptoms Post Flare
To cite this abstract in AMA style:
Mahmoud TG, Frits M, Iannaccone C, Bykerk VP, Bingham C III, Weinblatt M, Shadick NA. Correlates of Successful Flare Management: The Role of Clinician-Driven Treatment, Home-Based Strategies, and Medication Change [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/correlates-of-successful-flare-management-the-role-of-clinician-driven-treatment-home-based-strategies-and-medication-change/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/correlates-of-successful-flare-management-the-role-of-clinician-driven-treatment-home-based-strategies-and-medication-change/