Session Information
Date: Tuesday, November 15, 2016
Title: Metabolic and Crystal Arthropathies - Poster II: Epidemiology and Mechanisms of Disease
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Observational studies have reported that hyperuricemia may be protective in the development of osteoporosis. Serum urate concentrations positively correlate with bone density, and higher serum urate concentrations are associated with reduced risk of fragility fractures. The mechanisms of this bone-urate relationship are currently unexplained. The aim of this laboratory study was to examine whether soluble urate directly influences function of bone cells to promote bone formation.Methods:
For all assays, we examined the effects of soluble urate at physiological temperature and pH, at a range of urate concentrations consistent with those observed in humans (0 (control), 0.10, 0.20, 0.30, 0.40, 0.50, 0.60, 0.70 mmol/L). The effects of soluble urate on osteoclast development and function were examined using the RAW264.7 cell line osteoclastogenesis assay, a murine bone marrow osteoclastogenesis assay, a human peripheral blood osteoclastogenesis assay and a rat mature osteoclast assay. The early osteoblast-like MC3T3 cell line was used to examine the effects of soluble urate on cell viability (using MTT and alamarBlue assays), mineralisation, and gene expression for osteoblast differentiation markers. The MLO-Y4 osteocyte line was used to determine the effects of soluble urate on osteocyte viability and expression of genes implicated in osteocyte function.Results:
Addition of soluble urate in the RAW264.7 osteoclastogenesis assay led to small increases in osteoclast formation (ANOVA p=0.018, Figure). However, no significant effects on osteoclast number or activity were observed in the murine bone marrow assay, human peripheral blood osteoclastogenesis assay or rat mature osteoclast assay. In the MC3T3 osteoblast assays, soluble urate did not alter cell viability, mineralisation, or gene expression of markers including type 1 collagen, osteocalcin or osteoprotegerin. Similarly, in MLO-Y4 osteocyte assays, soluble urate did not alter cell viability or gene expression of RANKL, E11 or connexin-43.Conclusion:
Soluble urate at physiological concentrations does not promote anabolic bone formation pathways in in vitro bone cell assays. These data do not support the concept that the observed positive association between serum urate and bone density is due to direct effects of urate on bone. Figure: RAW264.7 osteoclastogenesis assays (showing pooled data from six biological repeats), demonstrating that higher concentrations of soluble urate leads to small increases in osteoclast formation. Dunnett multiple comparison test compared with control (no added urate) *p<0.05.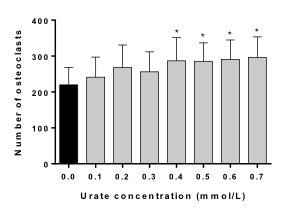 .
.
Disclosure: N. Dalbeth, None; B. Pool, None; A. Chhana, None; J. M. Lin, None; M. L. Tay, None; P. Tan, None; K. E. Callon, None; D. Naot, None; J. Cornish, None.
To cite this abstract in AMA style:
Dalbeth N, Pool B, Chhana A, Lin JM, Tay ML, Tan P, Callon KE, Naot D, Cornish J. Soluble Urate: A Direct Mediator of Bone Turnover? [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/soluble-urate-a-direct-mediator-of-bone-turnover/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/soluble-urate-a-direct-mediator-of-bone-turnover/
