Session Information
Session Type: ARHP Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: The United States (U.S.) is facing a significant deficit of physicians and rheumatology is subject to workforce challenges. Currently, in many areas in the U.S., persons with rheumatic disease face prolonged wait times and experience significant travel distances to a rheumatologist. Nurse Practitioners (NPs) and Physician Assistants (PAs), valuable members of the healthcare team, are utilized by about 25% of rheumatology practices. The 2015 ACR Workforce Study sought to expand current knowledge of the rheumatology workforce which included NP/PAs.
Methods: The 2015 ACR/ARHP Workforce Study was completed using several primary and secondary data sources, including ACR member data, state licensure registries, the 2005 ACR workforce study, professional organizations, and other medical literature. These data were augmented by a web-based survey to collect information on demographics, work settings, practice patterns, and retirement planning.
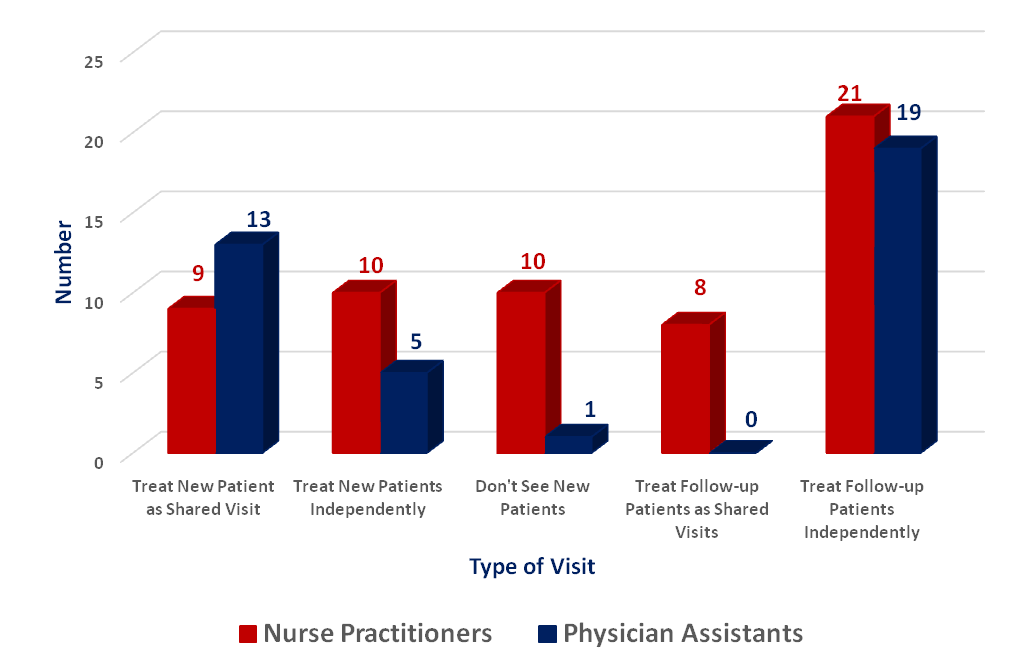
Results: Thirty-two completed survey responses were received (30% response rate; 32/110 NP/PA members), of which 23% were NPs (19/82) and 46% were PAs (13/28). Self reported as female were 54% (n=26) and 12.5% (n=6) as male, representative of the gender breakdown in the NP/PA professions. On average, NPs reported working 43 hours/week, while PAs reported working 39 hours/week. Of these hours, most were in clinical care (NP Mean=30 hours; PA Mean=27) with NPs reporting an average 31 patients and PAs an average 47 patients seen/week. A small percentage (<18% combined NP/PA) reported performing and billing for ultrasounds, DXA scans, and office based infusions. Although the majority of new patient visits seen by NP/PAs are shared visits with a rheumatologist, follow-up patients are mostly managed as independent visits (Figure 1). About 27% NPs/PAs plan to retire in the next 10 years. Of those, all plan to reduce their patient load before that time by 25-50%.
Conclusion: NP/PAs have been identified as a potential means of increasing the rheumatology workforce. While NP/PAs have different formal educational training, they function similarly within a rheumatology office and are able to accomplish unique needs of the practice, within the scope of state legal requirements. NPs and PAs offer one potential solution to meet rheumatology workforce needs particularly if use of this valuable resource is expanded and optimized. As the majority of NP/PA clinical encounters are follow-up visits accomplished “independently”, an opportunity to maximize the rheumatology workforce occurs when physicians, NPs and PAs function to the highest level of their licensure. Our data is limited only to NP/PA ARHP members and does not fully reflect NP/PAs in the rheumatology workforce. Recruitment and training strategies to increase the number of rheumatology NP/PAs to augment the workforce and improve access-to-care should be explored.
To cite this abstract in AMA style:
Smith BJ, Bolster MB, Ditmyer M, Jones KB, Monrad S, Battafarano D. Minding the Gap: the Use of Nurse Practitioners and Physician Assistants in U.S. Rheumatology Practice to Affect Rheumatology Workforce Shortages [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/minding-the-gap-the-use-of-nurse-practitioners-and-physician-assistants-in-u-s-rheumatology-practice-to-affect-rheumatology-workforce-shortages/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/minding-the-gap-the-use-of-nurse-practitioners-and-physician-assistants-in-u-s-rheumatology-practice-to-affect-rheumatology-workforce-shortages/