Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Antigenic triggers initiating granulomatous inflammation in giant cell arteritis (GCA) have yet to be elucidated. Recently, histopathological studies of temporal arteries from GCA patients have identified varicella zoster virus (VZV) antigen, implicating VZV as a potential causative organism. Given the cross-sectional design of past studies, the temporal relationship between herpes zoster (HZ) infection and GCA has not been established. Furthermore, if VZV is pathogenic, it is possible that HZ vaccination or antiviral treatments could prevent GCA. We assessed the associations of HZ, HZ treatment, and HZ vaccination with new onset GCA using two large administrative databases.
Methods: We utilized a random 5% sample of Medicare data (2006-2013) and the MarketScan Commercial Claims and Encounters database (2010-2014). Enrollees age >50 years with 365 days of continuous enrollment and without prior GCA or polymyalgia rheumatica were eligible for analysis. HZ events were identified by ICD-9 codes from hospital discharge or physician visits and classified as complicated (053.X, excluding 053.9) or uncomplicated (053.9). Antiviral treatments within 7 days of a HZ diagnosis were collected from pharmacy claims. HZ vaccination was identified through current procedural terminology and national drug codes. Incident GCA was defined by ICD-9 codes for GCA (446.5) from one hospital discharge or two physician visits 7 to 365 days apart. Using Poisson regression, we calculated GCA incidence stratified by HZ exposure. Cox proportional hazards regression was used to examine time-varying multivariable-adjusted associations of HZ, HZ treatment, and HZ vaccination with incident GCA.
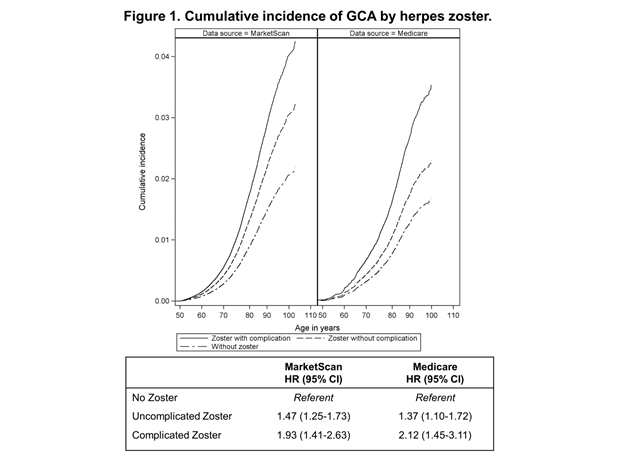
Results: A total of 16,664,161 persons were included (1,250,931 Medicare; 15,413,230 MarketScan) with 8,962 GCA cases (1,777 Medicare; 7,185 MarketScan) occurring over 37,993,079 pt-yrs of follow-up. GCA incidence was highest in those with complicated HZ in both datasets. Adjusting for age and sex, complicated HZ was associated with an ~2-fold increased risk while uncomplicated HZ was associated with a ~50% increased risk of GCA (Figure 1 table). The cumulative incidence of GCA stratified by HZ and adjusted hazard ratios (HR) are shown in Figure 1. Neither antiviral therapy (Medicare HR 0.70 [95% CI 0.48-1.03], MarketScan HR 1.15 [0.86-1.53]) nor HZ vaccination (HR 0.97, 95% CI 0.89-1.04) was associated with GCA.
Conclusion: HZ events are associated with an increased risk of GCA, with the highest risk amongst those with complicated HZ (e.g. cranial nerve involvement). These findings are among the first to establish a temporal relationship of prior HZ with subsequent GCA and provide further support for a potential causal association. We did not find evidence that either HZ vaccination or antiviral treatment is protective for GCA but additional study is warranted.
To cite this abstract in AMA style:
England BR, Mikuls TR, Xie F, Yang S, Chen L, Curtis J. Herpes Zoster and the Risk of Incident Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/herpes-zoster-and-the-risk-of-incident-giant-cell-arteritis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/herpes-zoster-and-the-risk-of-incident-giant-cell-arteritis/