Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Individuals with systemic lupus erythematosus (SLE) are frequently hospitalized. Determining factors associated with hospitalization rates may help to identify patients at highest risk for poor outcomes and improve healthcare resource utilization.
Methods: The Georgians Organized Against Lupus (GOAL) is a cohort of validated patients with SLE living in Atlanta, predominantly derived from the population-based Georgia Lupus Registry. Since 2011, participants are surveyed annually on sociodemographics, health insurance, the Self-Administered Brief Index of Lupus Damage (SA-BILD), and the Systemic Lupus Activity Questionnaire (SLAQ). Those with accumulation of any organ damage during the study period were deemed a Damage Progressor (DP). Patients were matched to the Georgia Hospital Discharge Database to capture all hospitalizations throughout the state from 2011 through 2013. Multivariable Poisson regression analyses were performed to explore the independent effect of demographic and disease-related factors on the hospitalization rate (HR), defined as the number of hospital admissions per 1000 person-years, and on the incidence rate ratio of hospitalizations.
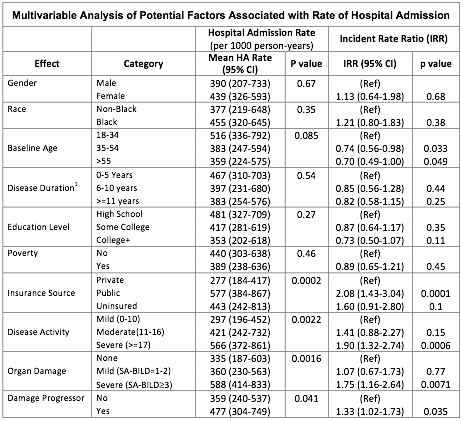
Results: 731 individuals were surveyed. 94% were female, 79% black, 35% had a high school education or less, and 45% lived below the Federal poverty level. Mean ages at SLE diagnosis and survey completion were 32.8 and 46.6 years, respectively, with mean disease duration of 13.8 years (±9.3) at the time of survey completion. 35% had private insurance, 47% public insurance (Medicare and/or Medicaid), and 17% were uninsured. Baseline self-reported disease activity was mild, moderate, and severe in 26%, 23%, and 50% of participants, respectively. While 25% had no organ damage at baseline, 38% had mild and 37% had severe damage. 345 individuals were hospitalized during the 3-year study period. The overall unadjusted HR per 1000 person-years was 668 and the HRs were 806 and 559 for those who were and were not a DP, respectively (p=0.01). The ratio of HRs for those who were DPs relative to those who were not DPs was 1.33 (95% CI: 1.02-1.73, P=0.04) after adjusting for confounders. Ages 18-34 at baseline, public insurance enrollment, severe disease activity, severe organ damage, and being a DP were independent predictors of increased HRs.
Conclusion: In this population-based cohort, nearly half were hospitalized over the 3-year study period. Notably, gender, race, education and poverty were not associated with increased hospitalizations. Our data suggest organ damage may increase the risk of hospitalizations with a 33% increased rate in DPs. Individuals enrolled in Medicare and/or Medicaid had over double the rate of hospitalizations compared to those with private insurance. The reasons for increased hospitalization with public insurance are unclear and should be explored further.
To cite this abstract in AMA style:
Lim SS, Bao G, Kan HJ, Pobiner B, Priest J, Eastman W, Easley K, Drenkard C. The Accumulation of Organ Damage, Public Insurance Enrollment and Youth Are Associated with Increased Hospitalizations in a Population-Based Cohort of Lupus Patient [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/the-accumulation-of-organ-damage-public-insurance-enrollment-and-youth-are-associated-with-increased-hospitalizations-in-a-population-based-cohort-of-lupus-patient/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-accumulation-of-organ-damage-public-insurance-enrollment-and-youth-are-associated-with-increased-hospitalizations-in-a-population-based-cohort-of-lupus-patient/