Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
Given the difficulties non-rheumatologists experience to early refer psoriasis patients at risk for Psoriatic Arthritis (PsA) we aim to explore patients experience of musculoskeletal symptoms and understand patients’ self-management of symptoms preceding the diagnosis of PsA through a qualitative study to provide a state of the art view on current medical practice eliciting room to improve early detection of PsA.
Methods:
A semi structured interview was developed based on the available literature and informal conversations with patients. The following data was collected from newly diagnosed PsA patients participating in the Dutch south wEst Psoriatic ARthritis cohort (DEPAR): medical history, physical load, previous and current joint and tendon complaints, general complaints, disabilities and emotional status and its influence on their daily life.
Results:
24 Newly diagnosed PsA patients (median age 52; 54% male; median duration of symptoms four years; 17% mono-, 21% oligo, 29% poly arthritis, 25% dactylitis, 4% axial and 8% enthesitis) participated in this study.
Patient at first did not involve their GP as they attributed their symptoms to physical exertion, obesity or other morbidity. If symptoms continued or worsened they involved their GP. Symptoms of the shoulders, wrists, back, hips and knees were first referred to physiotherapist or other specialists before they were seen by a rheumatologist, often taking years. While patients with hand symptoms were referred to the rheumatologist more quickly, as were patients with rapid accumulation of complaints.
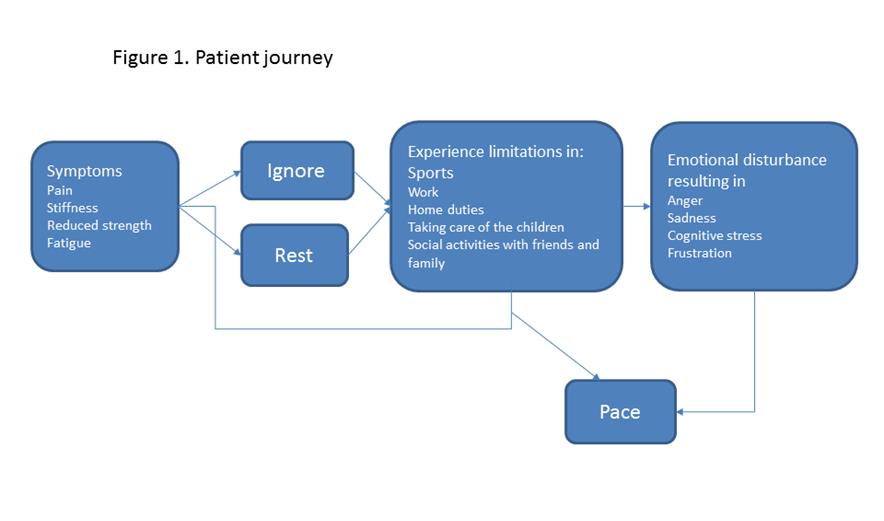
Figure 1 shows the different ways patients dealt with their symptoms before visiting the GP. Patients experience pain, stiffness, loss of strength and fatigue. Some patients decide to proceed with physical activity which often resulted in more pain and inability to perform daily activities. Some choose to avoid all physical activities that causes pain. And others choose to pace their activities. Ultimately, most of our patients ended up choosing for the latter. However, all patients experienced disability which often resulted in stress, frustration, sadness or anger.
Conclusion:
Patients and physicians are not alerted that symptoms of the large joints may be underlying PsA. Patients often first see physiotherapist and other specialist before they finally arrive at the rheumatologist. In the period preceding the diagnosis all patients struggle with pain and other symptoms impacting their daily life. Initially, they choose different coping strategies. While over time they all choose to pace their activities at the cost of losing wellbeing.
To cite this abstract in AMA style:
Rasappu N, Wervers K, Tchetverikov I, Kok MR, Gerards AH, Vis M, Luime JJ. Musculoskeletal Symptoms Preceding the Diagnosis of Psoriatic Arthritis – a Qualitative Exploration of the Patient Journey [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/musculoskeletal-symptoms-preceding-the-diagnosis-of-psoriatic-arthritis-a-qualitative-exploration-of-the-patient-journey/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/musculoskeletal-symptoms-preceding-the-diagnosis-of-psoriatic-arthritis-a-qualitative-exploration-of-the-patient-journey/