Session Information
Session Type: ACR Concurrent Abstract Session
Session Time: 4:30PM-6:00PM
Background/Purpose: Pneumocystis jiroveci (PJP) is an opportunistic infection associated with high mortality in patients with rheumatologic conditions. Given the paucity of data, clinical guidelines to initiate PJP prophylaxis are based on expert opinion and identify patients on >20 mg daily prednisone for >4 weeks duration for treatment. Herein we describe the PJP experience over a 20-year period at a single academic center.
Methods: We conducted a retrospective review of all patients admitted to a tertiary academic institution who received an ICD-9 code for Pneumocystis jiroveci (PJP) or Pneumocystis carinii (PCP) (136.3) from 1/1/1996-9/30/2015. Records were abstracted for clinical information including underlying disease, immunosuppressive regimen, lymphocyte count on admission, and outcome. Patients with underlying oncologic diagnoses or organ transplant history were excluded. Summary statistics were performed using Stata v.14.
Results: A total of 21 cases with confirmed PJP were reviewed, averaging to a rate of approximately one case per year. The most common underlying rheumatologic conditions with PJP infection were inflammatory myopathy, systemic lupus erythematosus (SLE), and granulomatosis with polyangiitis (GPA). None of these 21 patients was receiving PJP prophylaxis upon admission. The average time from rheumatologic disease diagnosis to PJP diagnosis was 50 ± 50 months. Data on duration of therapy prior to diagnosis were unavailable. All but three patients were lymphopenic upon presentation (absolute lymphocyte count 558 ± 449, range 40-1580, normal 1100-4800/mm3). Seventeen patients (81%) were receiving >20 mg prednisone at the time of diagnosis. Of the 4 who were receiving <20 mg prednisone, all received concomitant immunosuppressive medications, including 3 with cyclophosphamide (Table 1). For those patients with available lung function data (pulmonary function testing and/or high-resolution CT imaging, n=12), half had a history of ILD. There was a 43% (9/21) mortality rate overall.
Conclusion: PJP is a largely preventable complication of rheumatic disease treatment with a high mortality, and often occurs years after the initial rheumatologic disease is diagnosed. No patient developed PJP while on less than 20 mg prednisone monotherapy; however, lower doses were noted in those who developed PJP while on concomitant cyclophosphamide. While expert guidelines recommend PJP prophylaxis with patients on >20 mg prednisone for >4 weeks, consideration should be made for patients receiving any dose of prednisone who are also receiving cyclophosphamide, regardless of the underlying rheumatic disease. Table 1. Patients who developed PJP on less than 20 mg of prednisone 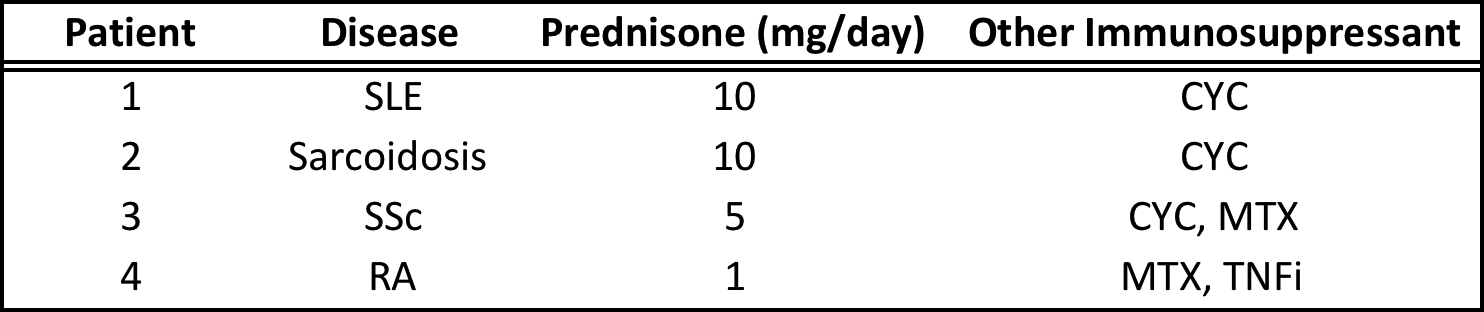
SLE = systemic lupus erythematosus, SSc = systemic sclerosis, RA = rheumatoid arthritis, CYC = cyclophosphamide, current or in past 12 months, MTX = methotrexate, TNFi = tumor-necrosis factor inhibitor, NR = not reported
To cite this abstract in AMA style:
Mecoli CA, Saylor D, Gelber AC, Christopher-Stine L. Pneumocystis Jiroveci in Rheumatic Disease: A 20 Year Single-Center Experience [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/pneumocystis-jiroveci-in-rheumatic-disease-a-20-year-single-center-experience/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/pneumocystis-jiroveci-in-rheumatic-disease-a-20-year-single-center-experience/
