Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Results From a Large International Inception Cohort. Jayne Little1, Mark Lunt1, Ben Parker1, Ian N. Bruce1 and The Systemic Lupus International Collaborating Clinics (SLICC) Group, 1Arthritis Research UK Centre for Epidemiology, Centre for Musculoskeletal Research, Institute of Inflammation and Repair, MAHSC, The University of Manchester, Manchester, United Kingdom
Background/Purpose: Glucocorticoids (GCs) are widely used in systemic lupus erythematosus (SLE). Whilst there is significant variability in how they are used, little is known about factors that explain this variability. We aimed to examine factors associated with oral GC use in a large international inception cohort.
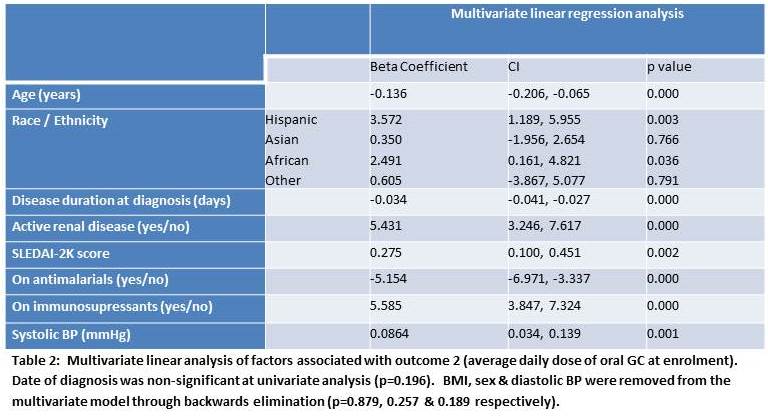
Methods: From 2000-11, we recruited patients within 15 months of developing four or more 1997 American College of Rheumatology (ACR) criteria for SLE. Data including disease characteristics and treatment were collected at enrolment and annually thereafter. Univariate analyses were performed to explore the cross-sectional relationship between predefined demographic and clinical (independent) variables and two measures of GC use at enrolment: 1) Taking oral GCs (yes/no) and 2) Current average daily dose of oral GCs (prednisolone equivalent). For each GC outcome, independent variables significant in univariate analysis (p<0.20) were entered into multivariate models using backwards selection to create the final models. Results: We studied 1700 patients at enrolment including 1506 (88.6%) women of whom 1189 (70.0%) were taking oral GCs at a median (IQR) dose of 20 (10-30) mg daily. Over the period of study recruitment (2000-11, there was no significant temporal trend in the proportion of patients taking GC at enrolment nor in the doses used. As can be seen in Tables 1 and 2, a number of factors were independently associated with GC use including male sex, younger age, the use of immunosupressants, renal disease and higher SLEDAI2K. In addition, race/ethnicity was independently associated with higher GC use. Compared to Caucasians, the OR (95%CI) for being on GCs were 3.32 (CI: 2.14-5.15), 6.56 (CI: 4.02-10.71) & 2.80 (CI: 1.96-4.01) for patients of Hispanic, Asian and African descent respectively (table 1). Hispanics and patients of African ancestry were taking an average (CI) 3.57 (1.19-5.96)mg and 2.49 (0.16-4.82)mg more GC per day than Caucasians respectively (table 2). 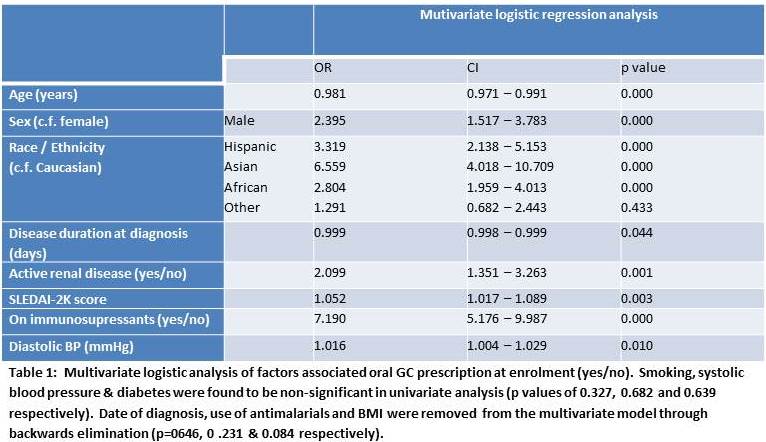
Conclusion: Standard of care therapy for SLE remains inadequate and over the period of study recruitment there was no significant change in how GCs were used in this cohort. A number of factors independent of disease activity and phenotype correlate with GC use and GC dose taken including race / ethnicity. A better understanding of the sources of this variation (including disease factors, socioeconomic factors, access to healthcare and physician and patient choice) may help to reduce GC use in SLE.
To cite this abstract in AMA style:
Little J, Lunt M, Parker B, Bruce IN. Predictors of Corticosteroid Use in the Systemic Lupus International Collaborating Clinics Inception Cohort – a Multivariate Analysis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/predictors-of-corticosteroid-use-in-the-systemic-lupus-international-collaborating-clinics-inception-cohort-a-multivariate-analysis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-corticosteroid-use-in-the-systemic-lupus-international-collaborating-clinics-inception-cohort-a-multivariate-analysis/