Session Information
Date: Tuesday, November 10, 2015
Title: Systemic Sclerosis, Fibrosing Syndromes and Raynaud's - Clinical Aspects and Therapeutics Poster III
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose : SSc related PH
carries a high mortality; with SSc-PH related to restrictive lung disease (RLD)
having worse prognosis and more rapid time to death.Speculation regarding potential
MMF anti-fibrotic and anti-remodeling effects on parenchymal lung and vascular
intimal fibrosis were supported by two prior large observational studies from
the US and the UK. Here, we analyzed predictive markers of mortality of SSc
patients with PH stratified for RLD and for MMF use in the prospective EUSTAR
database of > 12,000 SSc patients.
Methods : SSc patients with a registry
designation of elevated sPAP by either right heart catheterization (RHC) or, in
absence of RHC, by echocardiography were subsequently stratified by an FVC of
>70% or ≤ 70% predicted near the time of designationand by MMF use.
MMF <6 months or cyclophosphamide use were excluded. Calculations are
derived from one-way ANOVA. Categorical variables were
compared with Chi square. Comparison of survival was
done with Kaplan-Meier analysis.
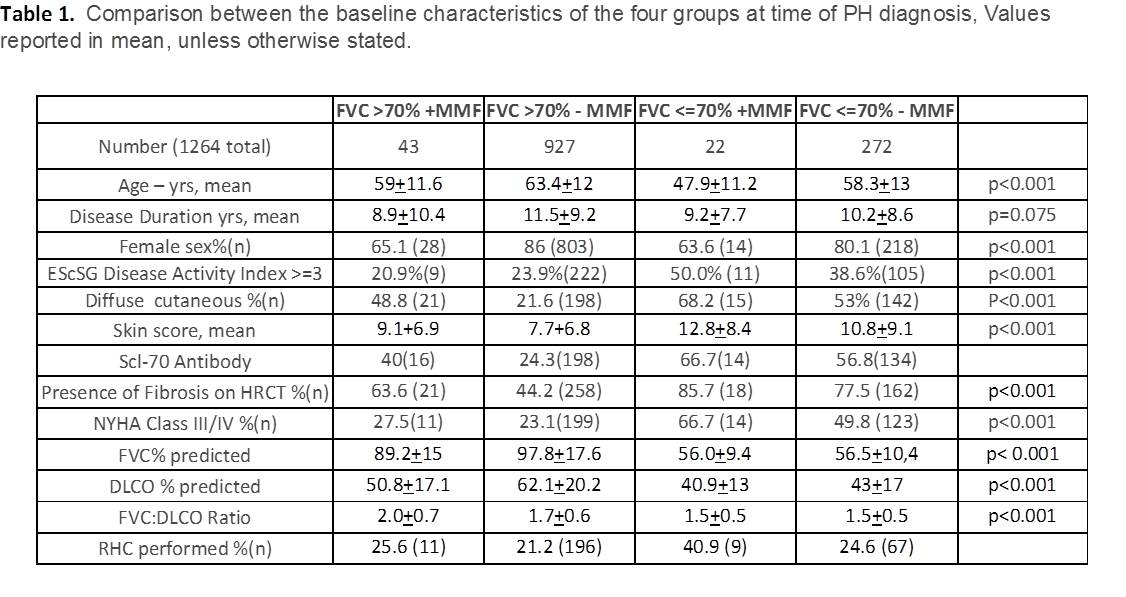
Results : Of 11,721 patients fulfilling ACR-EULAR
criteria, 1,264 matched criteria and had baseline FVC results coincident with
PH diagnosis, of those 965 had a baseline FVC of >70% with 43 on MMF and 927
without; and 294 had a baseline FVC≤70% with 22 on MMF and 272 without.
Overall, diagnosis was made by RHC in 263/1264 patients and in the remaining
patients by echo. There were no differences in disease duration. The FVC≤70
MMF+ was significantly younger with worse NYHA status and disease activity. In
the FVC≤70 (RLD) groups, FVC, DLCO and FVC:DLCO ratio were
significantly lower while the presence of fibrosis on HRCT and diffuse SSc
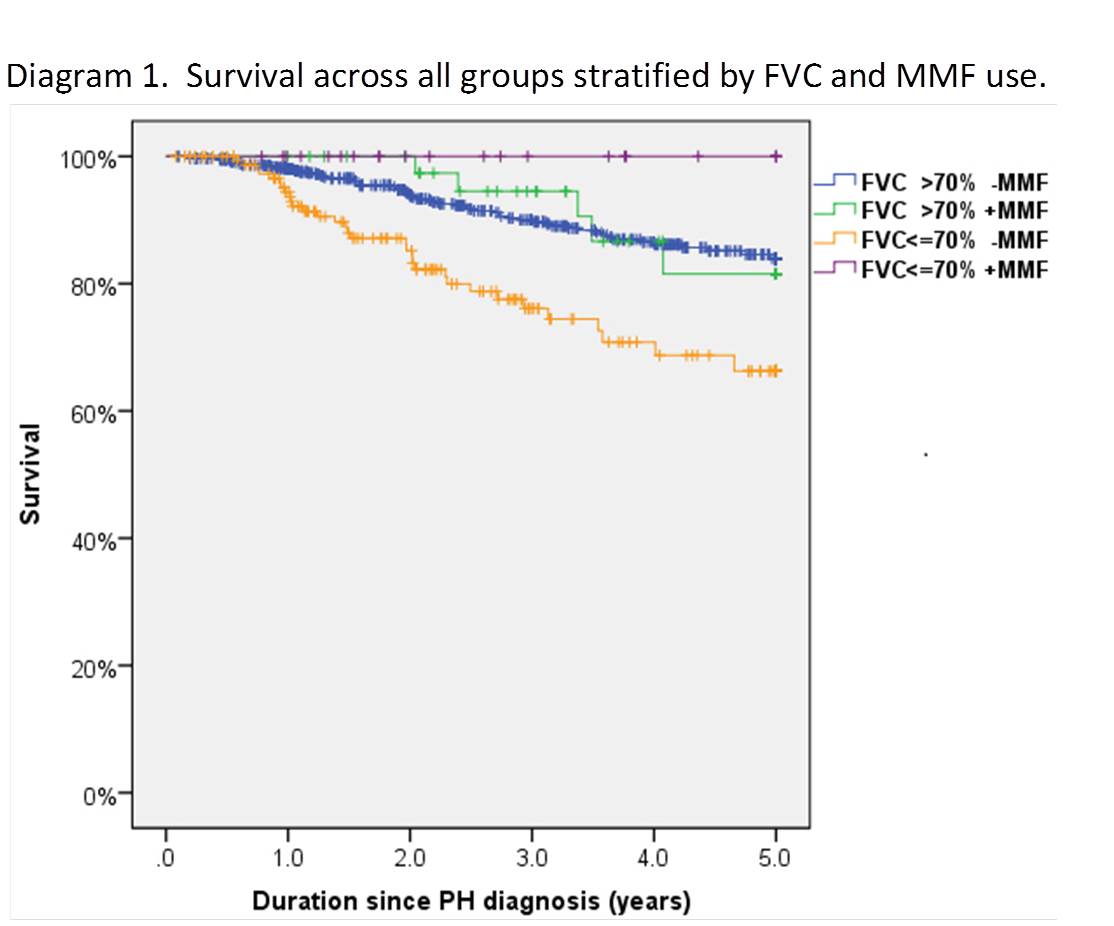
subtype were significantly higher. Survival assessed numerically and by Kaplan-Meier
analysis was significantly the worse in the FVC≤70 without MMF and
the best in the FVC≤70 with MMF across years 2 (p=0.001) and 3, 4, 5
years (p<0.0001) despite a significantly worse disease activity score and
NYHA class over the 4 groups.
Conclusion : Data trends in this registry
survey suggest MMF might be associated with beneficial survival in SSc PH. Limitations
of the study include mixed diagnostic methods of PH diagnosis given challenges
of accuracy of echocardiogram as well as inability to assess hemodynamics in
non-RHC diagnoses and therefore inability to assign WHO PH Group classification.
These findings warrant further analysis of international PH-SSc cohorts to
determine whether a prospective controlled trial may be developed to test the
mechanisms and impact of MMF in treating this important complication of SSc.
To cite this abstract in AMA style:
Saketkoo LA, Huscher D, Denton CP, Riemekasten G, Steen VD, Distler O. Mycophenolate Mofetil (MMF) Use in Systemic Sclerosis (SSc) Patients with a Designation of Elevated Systolic Pulmonary Artery Pressure (sPAP): Forced Vital Capacity (FVC), Outcomes and Survival from the European Scleroderma Trials and Research (EUSTAR) Database [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/mycophenolate-mofetil-mmf-use-in-systemic-sclerosis-ssc-patients-with-a-designation-of-elevated-systolic-pulmonary-artery-pressure-spap-forced-vital-capacity-fvc-outcomes-and-survival-from-t/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mycophenolate-mofetil-mmf-use-in-systemic-sclerosis-ssc-patients-with-a-designation-of-elevated-systolic-pulmonary-artery-pressure-spap-forced-vital-capacity-fvc-outcomes-and-survival-from-t/