Session Information
Session Type: ACR Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose:
Immunosuppressed patients are at higher
risk for infections compared to the general population. Vaccines decrease
morbidity and mortality, however vaccination status is not consistently
addressed in clinic. It has been shown that lack of physician recommendation
is a large barrier to vaccination. Pneumococcal vaccination is recommended for
patients with rheumatoid arthritis (RA) by the American College of Rheumatology
and Centers for Disease Control. The objective of this study was to evaluate
and improve the pneumococcal vaccination rate in RA patients at an urban
academic rheumatology clinic.
Methods:
A random sampling of 50 charts of
patients with a diagnosis of RA from July 2013 were reviewed to determine the
baseline pneumococcal vaccination rate. The rate was based on documentation in
the electronic medical record (EMR) vaccination status section. Subsequently,
3 focus groups with rheumatology providers, including physicians, nurses, and
medical assistants were conducted to discuss potential interventions to improve
the vaccination rate. Based on this feedback, a multi-faceted approach was
taken, including (1) an education program for providers regarding pneumococcal
vaccination for immunosuppressed patients, (2) adding vaccination status to the
EMR rheumatology note template, and (3) a pended order on patient’s arrival to
clinic. The protocol for the pended order begins with the medical assistant
who reviews the patient’s vaccination status and places a pended order if
unvaccinated. The physician discusses vaccination with the patient and signs
the order if in agreement, which is received by nursing who then administers
the vaccine. The signed order automatically records the vaccination date in the
vaccine section of the EMR. The vaccination rate for the post-intervention
period in May 2014 was then determined from a random sampling of 50 charts of
RA patients. The pre- and post-intervention rates were compared using a chi
square test.
Results:
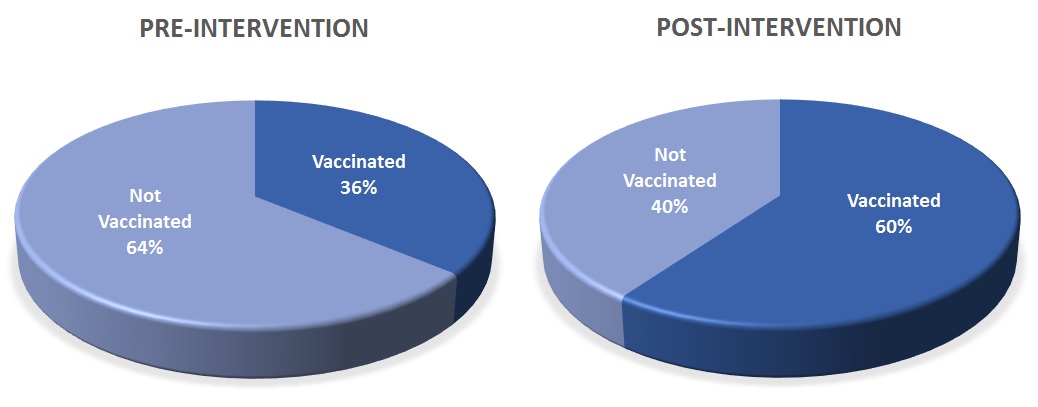
Age and gender demographics were similar
in pre-intervention (mean age 52 years, 84% female) and post-intervention (mean
age 57 years, 86% female) groups. The pneumococcal vaccination rate improved
from 36% pre-intervention to 60% post-intervention (p=0.016), see Figure
1.
Conclusion:
This multi-faceted approach led to a
statistically significant improvement in the pneumococcal vaccination rate in
RA patients. The pended order and pre-loaded vaccination status section in the
clinic note template both served as reminders for the physician to address
pneumococcal vaccination. The education program gave providers published
literature to support the decision to vaccinate. These processes have become
standard in our rheumatology clinics, and we plan to extend this work to
improve vaccination rates in all of our immunosuppressed patients.
Figure 1:
To cite this abstract in AMA style:
Reddy SB, Makris UE, Prescott K, Solow EB. Improved Pneumococcal Vaccination in Rheumatoid Arthritis Patients in an Urban Academic Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/improved-pneumococcal-vaccination-in-rheumatoid-arthritis-patients-in-an-urban-academic-rheumatology-clinic/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improved-pneumococcal-vaccination-in-rheumatoid-arthritis-patients-in-an-urban-academic-rheumatology-clinic/