Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose:
As rheumatologists search for new targets to improve immunosuppressive outcomes, the autonomic nervous system (ANS) as a co-factor in autoimmune disease expression has gained interest. At ACR 2014, heart rate variability (HRV), an accepted assessment of ANS state, was described as a biomarker in SLE. At ACR 2008, HRV predicted biologic treatment outcome for inflammatory arthritis in a 52-week, double-blind, prospective study1. But, how worthy is HRV as a metric with pathophysiologic and even therapeutic impact?
Methods:
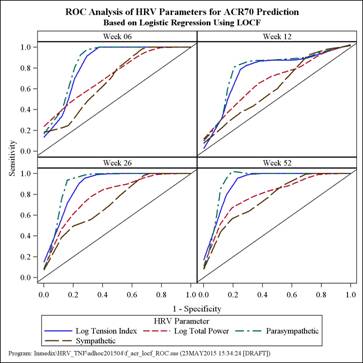
An in depth, post hoc analysis of the clinical study that established proprietary HRV (Omegawave Ltd, Espoo, Finland) as a predictor of biologic treatment outcome for inflammatory arthritis was conducted.1 To further evaluate the performance of HRV measures in predicting ACR outcomes, receiver operating characteristic (ROC) analysis have been carried out. Area under the ROC curve (AUC) was calculated and the ROC curve was plotted for each of the HRV measures. Youden index was used to find the optimal cutoff at which the sensitivity and specificity were maximized. Relative risk (RR) of the ACR response at the optimal cutoff was also calculated.
Results:
Thirty-three patients (25 rheumatoid and 8 psoriatic arthritis by ACR criteria) were included in the analysis.1 All HRV measures (parasympathetic, sympathetic, tension index, total power) achieved better prediction with increasing duration of anti-TNF therapy as measured by the AUC. The HRV measures provided moderate to high AUC values at week 26 and week 52 for ACR20/50/70 (range: 0.631 to 0.926). ROC AUC (95% CI) was most optimal for parasympathetic and log tension index to predict ACR70 response at 52 weeks at 0.926 (0.834, 1.000) and 0.918 (0.824, 1.000), respectively. At the optimal cutoff, sensitivity and specificity for the parasympathetic HRV measure to predict ACR70 at 52 weeks were 100% and 88.5%, respectively, and for the tension index, 100.0% and 84.6%, respectively. RR for all HRV measures at optimal cutoffs for ACR20/50/70 at 26 and 52 weeks ranged from 2.23 to infinity (all p-values < 0.05). Patients with parasympathetic > the optimal cutoff (0.17) were 16 times (RR 95% CI: 2.22 to 115.14) more likely to achieve ACR70 at 52 weeks than patients with parasympathetic ≤ the optimal cutoff (p-value < 0.001).
Conclusion:
Expanded statistical analyses of the referenced study further supports HRV as substantively impactful of prediction of anti-TNF biologic treatment outcome of inflammatory arthritis. These findings may encourage study in other diseases, with non-anti-TNF immunosuppressive regimens; expand elucidation of ANS immunomodulatory mechanisms that impact autoimmune disease expression and treatment response; and target the ANS as a prolific source of new therapeutics able to enhance immunosuppressive regimens.
- Autonomic Neurosci Basic Clinical 2008;143:58-67.
To cite this abstract in AMA style:
Holman A, Ng E. How Substantive Is Heart Rate Variability As a Predictor of Anti-TNF Treatment Outcome for Inflammatory Arthritis? [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/how-substantive-is-heart-rate-variability-as-a-predictor-of-anti-tnf-treatment-outcome-for-inflammatory-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-substantive-is-heart-rate-variability-as-a-predictor-of-anti-tnf-treatment-outcome-for-inflammatory-arthritis/