Session Information
Date: Monday, November 9, 2015
Title: Miscellaneous Rheumatic and Inflammatory Diseases Poster Session II
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Prior
studies of patients with rheumatic diseases admitted to ICU care have been
limited to case series; none included patients admitted after 2010. We examined
a modern cohort of rheumatic disease patients admitted to a tertiary care center
ICU. Given recent changes in the management of rheumatic diseases, we
hypothesized that infection would be a leading cause of mortality compared to mortality
from disease complications [e.g. interstitial lung disease (ILD), pulmonary
hypertension (PH)].
We
queried the University of California, San Francisco electronic health record
(EHR) to identify patients with rheumatic disease and an ICU admission between
6/13/2012-6/5/2015. We included patients with an ICD9 code for 1 of 11
rheumatologic diagnoses listed among admission diagnoses, hospital-problem
lists, discharge diagnoses, or billing data for the encounter. We assessed
in-hospital mortality (primary outcome) and other covariates including reason for
ICU admission and immunosuppressive use via chart review of the EHR by 1 author.
ICU encounters following elective surgeries, for the sole purpose of medication
titration, or for the primary reasons of myocardial infarction and arrhythmia
were excluded. The primary outcome was in-hospital mortality. EHR chart review
was performed to confirm diagnoses, determine the cause of ICU admission, and identify
immunosuppressive use.
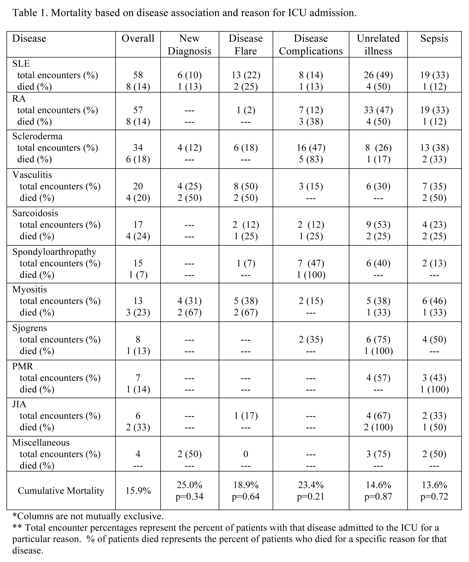
239
ICU encounters for 204 patients were identified. Diagnoses are listed in the
Table. 37 (15%) of encounters resulted
from primary rheumatic disease flare, 48 (20%) from disease complications (e.g.
ILD, PH), and 109 (46%) from presumably unrelated medical illnesses. 81 (34%) encounters
were caused or complicated by sepsis. Overall in-hospital mortality for this
cohort was 15%, with higher mortality among patients with a new rheumatic
disease diagnosis made during that same admission (25%) and disease
complications (23%), although these did not reach statistical significance. Additional
results are shown in the Table. Sepsis-related mortality was
not higher in patients receiving significant immunosuppression (10%, p=0.77)
defined as prednisone > 15 mg/day or the use of another cytotoxic agent.
To
our knowledge, this is the largest study of patients with rheumatic disease admitted
to the ICU. Compared with prior studies,
this cohort had lower overall mortality (16% vs. 17-55% in prior reports), and
infection was not the major cause of in-hospital death. Additional analyses are required to control
for potential confounders. In the future, we plan to investigate the
performance of traditional markers of ICU mortality ( e.g.
APACHE scores, vasopressors, ventilation) in this cohort and expand these
methods (automated extraction of structured and unstructured (text) data) to
construct a registry of critically ill rheumatic disease patients to guide
future research.
To cite this abstract in AMA style:
Wilfong EM, Murray SG, Schmajuk G, Yazdany J. Death and Infection Rates Appear Reduced in a Modern Cohort of ICU Patients with Rheumatic Disease [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/death-and-infection-rates-appear-reduced-in-a-modern-cohort-of-icu-patients-with-rheumatic-disease/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/death-and-infection-rates-appear-reduced-in-a-modern-cohort-of-icu-patients-with-rheumatic-disease/