Session Information
Date: Sunday, November 8, 2015
Title: Epidemiology and Public Health I: RA Comorbidities and Mortality
Session Type: ACR Concurrent Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: Suboptimal use of secondary
preventive pharmacotherapies after acute coronary syndrome (ACS) in patients
with rheumatoid arthritis (RA) has been suggested to contribute to an increased
risk of deaths and recurrent events following ACS. The objectives of this study
were therefore to investigate whether (i) use of
secondary preventive pharmacotherapies, (ii) long term mortality risk and (iii)
risk of recurrent ACS after incident ACS differ in patients with prevalent RA
and compared to general population comparators.
Methods: Using the Swedish national patient
register, patients with prevalent RA and matched general population comparators
with incident ACS between 2007 and 2010 were identified. After the ACS,
information on dispensed secondary preventive drugs (antiplatelets,
β-blockers, statins and RAS-blockers) was retrieved from the prescribed
drug register and analyzed during 4 consecutive time periods the year following
the ACS. Information on deaths and recurrent ACS was also retrieved and
analyzed at 1 year and complete follow-up period, until the end of 2011, using
cox regression models stepwise adjusted for preexisting comorbidities and
ACS-type.
Results: 1135 (0.9%) of the RA-patients and
3184 (0.5%) of the comparators were listed with an incident ACS between 2007 and
2010 and remained eligible for analysis as exposed cases (RA-cases) and
unexposed cases (Population-cases) . Among cases diagnosed with transmural
myocardial infarction (MI), there were no differences in dispensed drugs within
any of the time periods studied. Among RA-cases diagnosed with subendocardial and unspecific MI, the proportion dispensed antiplatelets were lower compared to population-cases within
the first two time periods studied, but during the last two time periods these
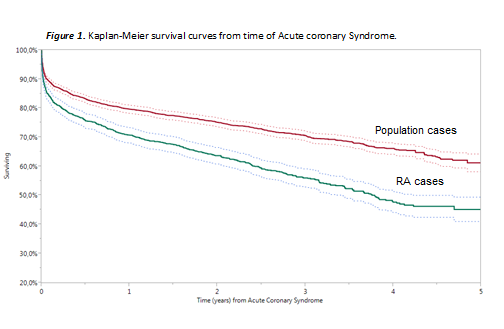
discrepancies disappeared. RA-cases had higher case-fatality rates the year
following the ACS and during the complete follow-up period. The relative
mortality risk was increased by 60% at 1 year (HR1.59 [95% CI 1.39-1.82]) and
70% during the complete follow-up period (HR 1.73 [95% CI 1.55-1.93]). RA-cases
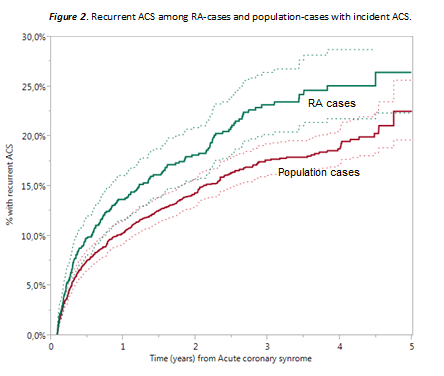
also had higher recurrence rates at 1 year and during the complete follow-up
period, corresponding to an increased relative risk of approx. 30% (1 year HR
1.35 [95% CI 1.09-1.68]; Follow-up HR 1.34 [95% CI 1.12-1.60]), which remained
stable after adjusting for previous comorbidities and infarct-type.
Conclusion: Despite similar usage of secondary
preventive pharmacotherapies, patients with prevalent RA suffer increased risk
of recurrent events and death after ACS compared to general population
comparators.
To cite this abstract in AMA style:
Mantel , Holmqvist M, Jernberg T, Wållberg-Jonsson S, Askling J. Secondary Preventive Pharmacotherapy and Longterm Outcomes Following Acute Coronary Events in Patients with Prevalent Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/secondary-preventive-pharmacotherapy-and-longterm-outcomes-following-acute-coronary-events-in-patients-with-prevalent-rheumatoid-arthritis/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/secondary-preventive-pharmacotherapy-and-longterm-outcomes-following-acute-coronary-events-in-patients-with-prevalent-rheumatoid-arthritis/