Session Information
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Patients with established RA undergoing total joint arthroplasty (TJA) frequently experience a disease flare within 6 weeks of surgery. This study aims to determine which histopathologicfeatures indicating active synovial inflammation in tissue obtained during TJA was associated with patients who experience post-op flare.
Methods: Synovial tissue obtained at the time of TJA from a cohort of well-characterized RA patients was examined by 2 experienced musculoskeletal pathologists for features known to be associated with rheumatoid arthritis. Significant previously described synovial pathologic features selected by unadjusted logistic regression included synovial lymphocytic and plasma cell infiltration, sclerosis/fibrosis, synovial lining hyperplasia, vascularity, and mucoid change were combined as a limited pathology score. Patient’s summary scores were compared to clinical status, including flare yes/no whether in the 6 week postoperative course. Inter-pathologist reliability, along with disease characteristics and flare status correlations, were assessed using Spearman’s correlation coefficient. Flare was classified using patient self-report and MD agreement based on chart review. Immunohistochemicalstaining for Rho Kinase pathway markers was performed.
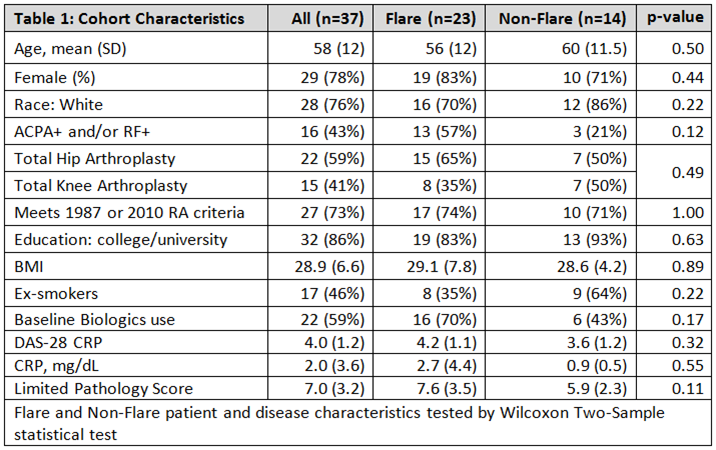
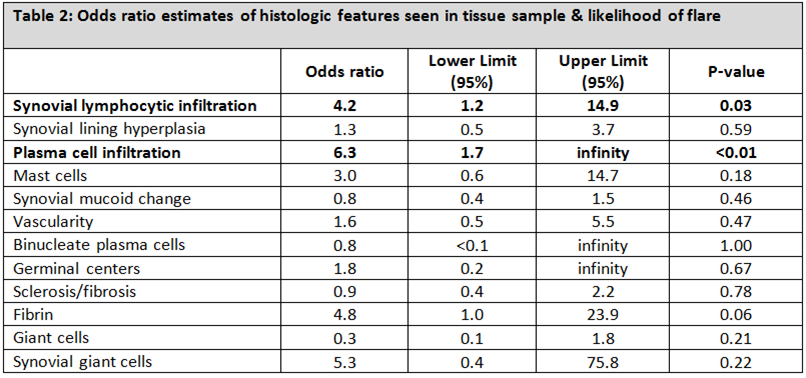
Results: Baseline and disease characteristics from 37 RA patients showed no differences in those who reported flare (n=23) vs. those who did not (n=14) (Table 1). Pathologist scoring of summed synovial inflammatory features were highly correlated between (Spearman’s rho=.55, p-value=0.01) and within (Spearman’s rho=0.7, p<0.01) readers. While there was no correlation between the summary pathology score and baseline disease characteristics (DAS28CRP/flare: rho=0.2, CRP/ flare: rho=0.2) , flare was associated with synovial lymphocytic infiltration (OR 4.2, 95% CI 1.2-14.9, p=0.03), and plasma cell infiltration (OR 6.3, 95%CI 1.7- ∞, p<0.01). Sclerosis/fibrosis was not significantly associated with flare (OR 0.9, 95%CI 0.4-2.2, p=0.78) (Table 2). The pERM staining (surrogate marker for ROCK activation) could be observed in different cellular components but the staining pattern did not differentiate flarers.
Conclusion: Inflammatory histological features in synovial tissue at the time of surgery are associated with a higher risk for post-operative flare. The notion that RA at the time of arthroplastyrepresents “burnt-out disease” should be re-evaluated.
This study was supported by the Clinical Translational Science Center (CTSC) (UL1-TR000457-06)
To cite this abstract in AMA style:
Goodman SM, Friedlander R, Figgie C, Pernis AB, Rozo CT, Gravallese EM, DiCarlo EF, Donlin LT, Figgie MP, Khianey R, Hoang A, Andersen K, Chowdhury L, Bykerk V. Histologic Scoring of Arthroplasty Synovial Samples May Predict RA Flare [abstract]. Arthritis Rheumatol. 2015; 67 (suppl 10). https://acrabstracts.org/abstract/histologic-scoring-of-arthroplasty-synovial-samples-may-predict-ra-flare/. Accessed .« Back to 2015 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/histologic-scoring-of-arthroplasty-synovial-samples-may-predict-ra-flare/