Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose:
Rheumatoid Arthritis (RA) is highly associated with the production of autoantibodies, including rheumatoid factors and anti-citrullinated protein antibodies (ACPA). It remains uncertain whether production of autoantibodies in RA results from a failure of peripheral B cell deletion or anergy, or from augmented T helper cell-induced differentiation. Unfortunately, our ability to directly study pathogenic B cells in RA has been hampered by their relatively low numbers in peripheral blood and our inability to directly monitor their antigen specificity.
Methods:
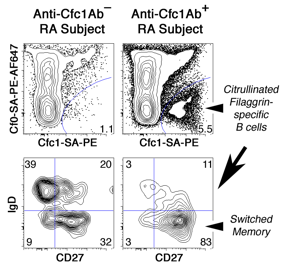
We now report the development of a B cell “antigen tetramer” system for use with multiparameter flow cytometry that can accurately detect and phenotype self antigen-specific B cells in RA patients. Arginine-312 —> Citrulline substituted filaggrin cyclic peptide 306-324 (Cfc1) was biotinylated and multimerized using streptavidin (SA)-phycoerythrin (PE) conjugates. A “decoy tetramer” was also created using SA-PE-Alexa Fluor 647 (AF647) conjugates and biotinylated native filaggrin cyclic peptide (Cf0) to facilitate exclusion gating of B cells that bind native filaggrin, biotin, SA, or PE.
Results:
46% of tested subjects in our University of Minnesota ACPA+ RA cohort demonstrated IgG anti-Cfc1 antibodies by ELISA (>95% specificity threshold). Using a combination of the Cfc1 and Cf0 antigen tetramers and flow cytometry, we observed in RA patients that lack Cfc1 Ab (n=22) a low number of Cfc1-specific PBMC B cells (49±31 per million) that was similar to healthy controls (HC) (51±29, n=9). Nevertheless, Cfc1-binding B cells in anti-Cfc1 Ab- RA subjects more frequently demonstrated a CD19+CD20+IgD-CD27+ phenotype consistent with isotype switching and memory cell differentiation (35±15%) as compared to either randomly selected PBMC B cells from the same patient (18±8%; p<0.01) or Cfc1-binding B cells in HC (16±11%; p=0.02). Anti-Cfc1 Ab+ RA subjects (n=21) demonstrated both an increased frequency of Cfc1-binding B cells (125±85 per million; p=0.02 vs. HC, p=0.01 vs. anti-Cfc1 Ab- RA) and increased proportion having a switched memory phenotype (55±18%; p<0.01 vs. both HC and anti-Cfc1 Ab- RA). Among all ACPA+ RA subjects tested, the level of anti-Cfc1 Ab predicted the frequency of switched memory Cfc1-binding B cells in PBMC (r2=0.38).
Conclusion:
The loss of B cell tolerance to citrullinated filaggrin and production of anti-Cfc1 autoantibodies in RA is associated with an expanded population of Cfc1 tetramer-binding switched memory B cells in the PBMC. Use of antigen tetramers to positively identify and characterize antigen-specific B cells will accelerate the investigation of pathogenic B cells in autoimmune disease and holds promise as a valuable biomarker system for use in human therapeutic trials.
Disclosure:
P. Titcombe,
None;
L. O. Barsness,
None;
L. Giacobbe,
None;
E. Baechler Gillespie,
None;
E. J. Peterson,
None;
D. L. Mueller,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/production-of-citrullinated-filaggrin-specific-igg-in-rheumatoid-arthritis-patients-is-associated-with-an-expansion-of-citrullinated-filaggrin-tetramer-binding-switched-memory-blood-b-cells/