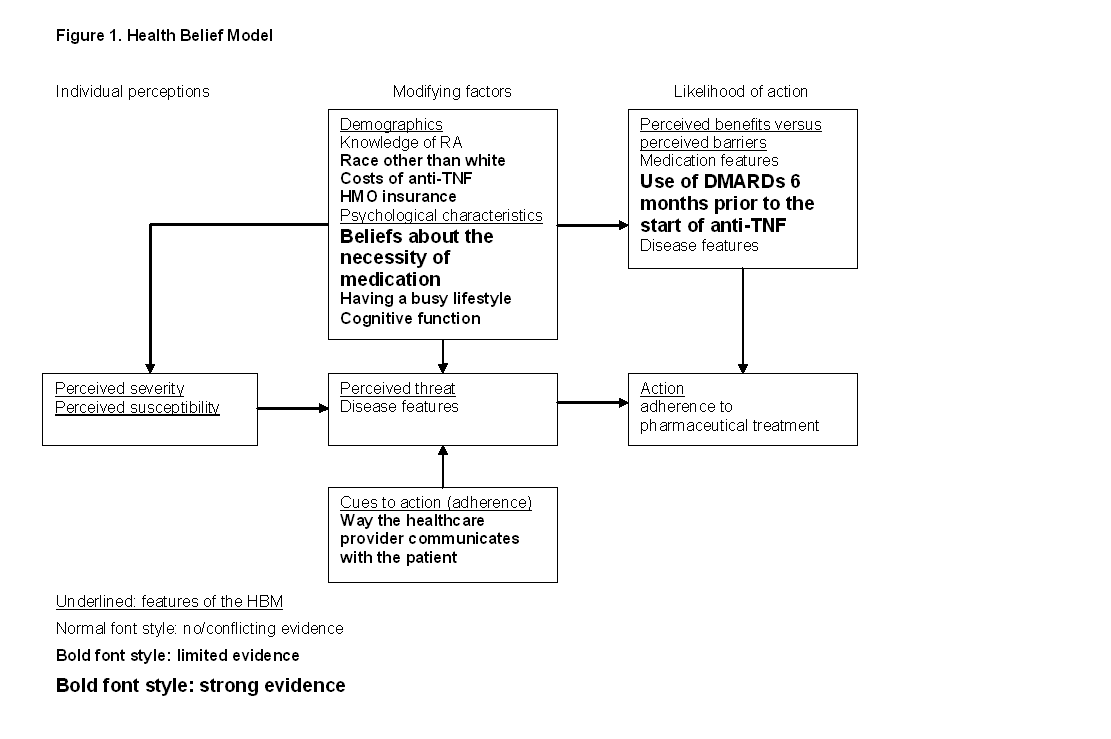
In the early stages of Rheumatoid Arthritis (RA), adherence to the prescribed treatment is important to prevent irreversible joint damage. However, medication adherence rates in RA patients can be improved. To explain the suboptimal adherence, factors that influence adherence should be elucidated. These factors were last reviewed in 1982. Since then, treatment strategies for RA have changed, which means that nowadays different factors might play a role. Our aim is therefore to review adherence rates reported in the literature, to identify factors associated with adherence, to review the strength of the association between these factors and adherence and to cluster the identified factors according to the Health Belief Model (HBM) (figure 1.).
Methods:
PubMed, PsycINFO, EMbase and CINAHL databases were systematically searched from inception to February 2011. Articles were included if they addressed medication adherence, used a reproducible definition, determinants and its statistical relationship. Methodological quality was assessed using a quality assessment list for observational studies derived from recommendations from Sanderson, Tatt and Higgins (2007). The strength of evidence for factors associated with adherence was assessed by defining 5 levels of evidence. Resulting factors were interpreted using the HBM.
Results:
18 out of the 1479 identified studies remained. Adherence rates ranged between 49.5% and 98.5%. 64 factors were identified and grouped according the HBM into demographic and psychosocial characteristics, cues to action and perceived benefits versus perceived barriers. The belief that the medication is necessary and DMARD use prior to the use of anti-TNF had strong evidence for a positive association with adherence. There is limited evidence for positive associations between adherence and race other than White, general cognition, satisfactory contact with the healthcare provider and the provision of adequate information from the healthcare provider. There is limited evidence for negative associations between adherence and having HMO insurance, weekly costs of TNF-I, having a busy lifestyle, receiving contradictory information or delivered information in an insensitive way by the rheumatologist. 18 factors were unrelated to adherence. The results are presented in figure 1.
Conclusion:
The strongest relation with adherence is found for prior use of DMARDs before using anti-TNF and beliefs about medication. Because the last one is modifiable, this provides hope to improve medication adherence. Since research on factors influencing adherence has mostly focussed on demographic and disease futures, future studies should use a theoretical framework to explore the role of interpersonal and other relevant factors.
Disclosure:
A. Pasma,
None;
A. van ‘t Spijker,
None;
J. van Busschbach,
None;
J. M. W. Hazes,
None;
J. J. Luime,
None.
« Back to 2012 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/what-will-determine-adherence-to-pharmaceutical-treatment-for-rheumatoid-arthritis-a-systematic-review/